Smoking Cessation Drug Adjustment: What Works and What to Watch For
When you're trying to quit smoking, the right smoking cessation drug adjustment, the process of changing dosage, timing, or type of medication to match your body’s response and reduce withdrawal symptoms. Also known as quit smoking medication titration, it’s not just about picking a drug—it’s about tuning it to your life. Many people start with nicotine patches or gum, only to find they still crave cigarettes. That’s not failure. It’s a signal that the dose or type needs tweaking.
Three main drugs are used to help people quit: nicotine replacement therapy, products like patches, lozenges, or inhalers that deliver controlled doses of nicotine without smoke, varenicline (Chantix), a pill that blocks nicotine’s effect on the brain while reducing cravings, and bupropion (Zyban), an antidepressant that helps ease withdrawal by affecting brain chemicals linked to addiction. Each works differently. Nicotine replacement fixes the physical craving. Varenicline targets the brain’s reward system. Bupropion helps with mood and focus. Mixing them isn’t always better—sometimes it’s just about getting the dose right.
Adjusting these drugs isn’t just about increasing the dose. It’s about timing. Maybe your patch isn’t lasting long enough. Maybe your varenicline makes you feel sick in the morning but works fine at night. Maybe you’re still reaching for a cigarette after meals because the bupropion hasn’t built up in your system yet. These aren’t random setbacks. They’re clues. People who adjust their meds based on when cravings hit—like right after coffee or during stress—have higher success rates than those who stick rigidly to the label.
Side effects matter too. Nausea from varenicline? Try lowering the dose for a week and building up slowly. Dry mouth from nicotine gum? Switch to patches. Trouble sleeping with bupropion? Take it before noon. These aren’t reasons to quit the plan—they’re signals to tweak it. And yes, some people need to switch drugs entirely. If one doesn’t work after 4–6 weeks, trying another isn’t giving up. It’s smart.
What you won’t find in most guides is how often people stop because they think the drug isn’t working—when really, they just didn’t adjust it. A 2023 study of over 12,000 quitters found that those who adjusted their medication within the first two weeks were 3 times more likely to stay smoke-free after six months. That’s not luck. That’s precision.
You don’t need a doctor to start adjusting—though talking to one helps. But you do need to pay attention. Keep a simple log: what you took, when you took it, when cravings hit, and how bad they were. That’s the data that tells you what to change. No apps needed. Just pen and paper.
Some people think quitting smoking is about willpower. It’s not. It’s about chemistry. And chemistry changes. Your body adapts. Your triggers shift. Your meds need to keep up. A smoking cessation drug adjustment isn’t a sign you’re failing. It’s the smartest thing you can do to finally succeed.
Below, you’ll find real-world guides on how people have adjusted their quit-smoking meds—what worked, what didn’t, and how they kept going even when the first try fell short.
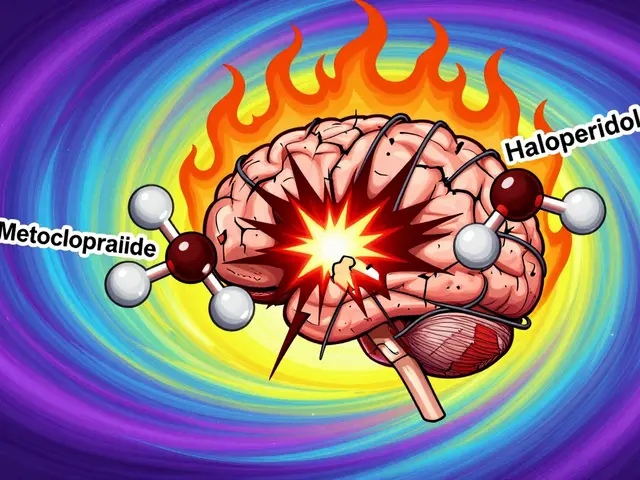
How Smoking Changes How Your Medications Work: Enzyme Induction and Drug Levels
Smoking changes how your body processes medications by boosting liver enzymes, making some drugs less effective. When you quit, those same changes can cause dangerous toxicity. Know which meds are affected and how to adjust safely.