Central Sleep Apnea: Causes, Risks, and What Medications Can Help
When your brain forgets to tell your body to breathe, you're dealing with central sleep apnea, a breathing disorder where the brain fails to send proper signals to the muscles that control breathing during sleep. Also known as neurogenic sleep apnea, it's not caused by blocked airways like obstructive sleep apnea—it's a communication breakdown between your brain and lungs. This isn't just about snoring or feeling tired. It’s about your body going minutes without oxygen while you sleep, often without you ever waking up to notice.
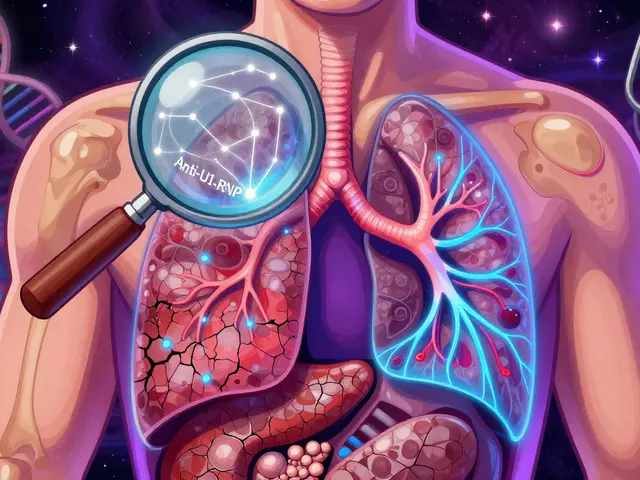
People with heart failure, stroke, or those on long-term opioid pain meds are most at risk. oxygen therapy, a treatment that delivers supplemental air to maintain blood oxygen levels during sleep is often used, but it doesn’t fix the root problem. CPAP alternatives, devices like ASV or adaptive servo-ventilation that adjust pressure based on breathing patterns are more targeted, helping retrain the brain’s breathing rhythm. Unlike regular CPAP machines that push air through a blocked airway, these devices respond to actual pauses in breathing signals—making them critical for true central apnea cases.
Medications rarely cure central sleep apnea, but some can help manage it. Acetazolamide, a diuretic originally used for altitude sickness, has been shown to stimulate breathing in some patients. Theophylline, an old asthma drug, is sometimes prescribed off-label for its respiratory stimulant effects. But these aren’t magic pills—they work best alongside device therapy and only under close medical supervision. What’s more, opioid use is a major trigger, and tapering off these drugs under a doctor’s care can sometimes reverse the condition entirely.
What you won’t find in most online guides is how often central sleep apnea is misdiagnosed as obstructive sleep apnea. If you’ve tried CPAP and still wake up gasping, exhausted, or with headaches, it might not be your throat—it could be your brain. That’s why knowing the difference matters. Your treatment plan changes completely depending on the type.
The posts below cover real-world cases, drug interactions to watch for, and how sleep disorders connect to heart health, kidney function, and even medication adherence. You’ll find guides on how to track symptoms, what to ask your doctor before starting a new sleep device, and how some of the same drugs used for diabetes or blood pressure can accidentally make central apnea worse. This isn’t theoretical—it’s what people are dealing with right now, and the solutions are more practical than you think.
Opioids and Sleep Apnea: How Opioids Trigger Dangerous Breathing Problems During Sleep
Opioids can severely worsen sleep apnea by suppressing breathing signals in the brain, leading to dangerous pauses in breathing during sleep. Learn how this happens, who's at risk, and what to do to stay safe.