Hormone Replacement: What It Is, Who Needs It, and What You Should Know
When your body stops making enough of certain hormones, things like energy, mood, sleep, and even your sex drive can go off track. Hormone replacement, a medical treatment that adds back hormones your body no longer produces in sufficient amounts. Also known as hormone therapy, it’s not just for menopause—it’s used for low testosterone, thyroid problems, adrenal insufficiency, and more. This isn’t about chasing youth or quick fixes. It’s about fixing real imbalances that affect how you feel every day.
For women, estrogen, a key female hormone that drops sharply after menopause is often the main focus. Hot flashes, night sweats, vaginal dryness, and brain fog aren’t just annoying—they can make daily life hard. Hormone replacement can ease these symptoms, but it’s not one-size-fits-all. Some women take estrogen alone; others need progesterone too, especially if they still have a uterus. For men, testosterone, the primary male hormone that declines slowly with age can drop low enough to cause fatigue, muscle loss, depression, or trouble getting an erection. Testing is key—symptoms alone aren’t enough to start treatment.
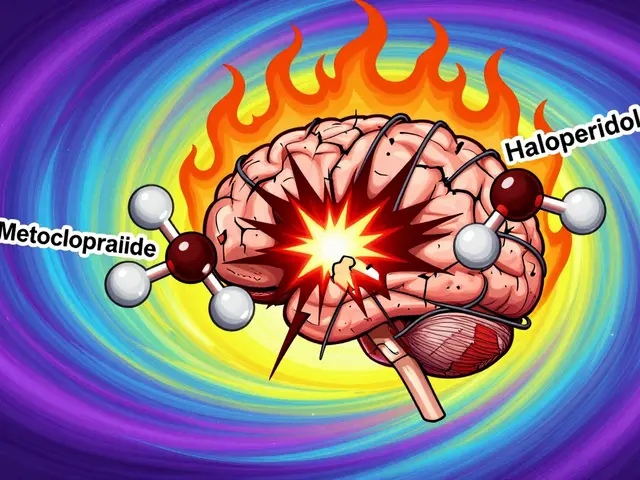
It’s not all simple. Hormone replacement can interact with other meds. For example, if you’re on blood thinners like warfarin, or taking antidepressants, your hormone levels might change how those drugs work—or vice versa. Smoking affects how your body breaks down hormones, and so do certain antibiotics like rifampin. Even supplements can interfere. That’s why working with a doctor who understands your full health picture matters more than just getting a prescription. You don’t need to suffer through mood swings or exhaustion just because you’re aging. But you also don’t want to jump into hormone therapy without knowing the risks, like increased chances of blood clots, breast cancer, or liver issues in rare cases.
What you’ll find below isn’t a sales pitch. It’s a collection of real, practical posts from people who’ve been there—whether they’re managing menopause with hormone therapy, dealing with side effects from testosterone, or trying to understand why their doctor changed their dose after a lab test. Some posts dig into drug interactions, like how rifampin can make birth control fail by speeding up hormone breakdown. Others talk about how smoking alters how your body processes meds. There’s even advice on tracking symptoms and working with your pharmacist to avoid hidden risks. This isn’t theory. It’s what works, what doesn’t, and what to watch out for when your body’s chemistry shifts.
Compare Estrace (Estradiol) with Alternatives: What Works Best for You
Estrace (estradiol) helps with menopause symptoms, but it's not the only option. Compare tablets, patches, vaginal treatments, and non-hormonal alternatives to find what works best for your body and lifestyle.