Estradiol: What It Is, How It Works, and What You Need to Know
When your body starts producing less estradiol, the primary form of estrogen that regulates reproductive health, bone density, and mood. Also known as 17-beta-estradiol, it's the hormone your ovaries make before menopause — and what many women replace with therapy to ease hot flashes, night sweats, and vaginal dryness. It’s not just about comfort. Low estradiol levels can weaken bones, raise heart disease risk, and even affect memory. That’s why understanding how it works — and when to treat low levels — matters more than most people realize.
Many people confuse estradiol with other estrogens like conjugated equine estrogen (CEE), but they’re not the same. Estradiol is bioidentical, meaning it matches the molecule your body naturally makes. That’s why it’s often preferred over older synthetic versions in hormone replacement therapy. It’s available as pills, patches, gels, and even vaginal rings — each with different absorption rates and side effect profiles. For example, patches avoid the liver’s first-pass effect, which lowers the risk of blood clots compared to oral forms. And while some think all estrogen therapy is risky, studies show that for healthy women under 60 starting treatment near menopause, the benefits often outweigh the risks — especially when used at the lowest effective dose.
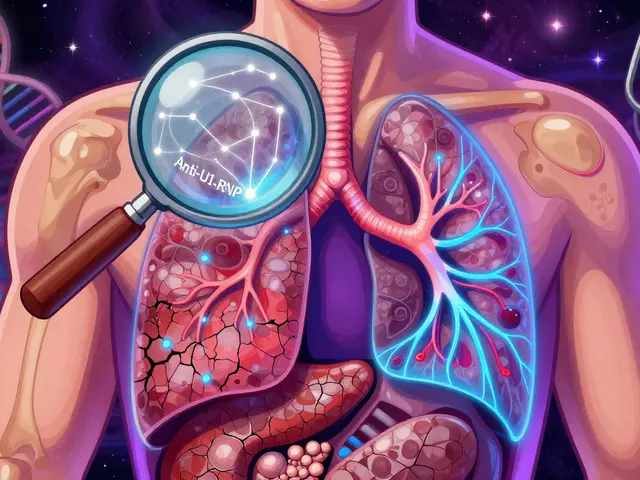
But estradiol doesn’t work in isolation. It interacts with other hormones like progesterone, which is why women with a uterus need to take both to protect against uterine cancer. It also affects how your body handles other drugs. For instance, estradiol can change how warfarin works, requiring more frequent INR checks. It can also influence thyroid medication needs or make some antidepressants less effective. And if you’re taking it for menopause, you’ll want to watch for signs of too much — like breast tenderness, bloating, or mood swings — because those often mean your dose is too high.
What’s surprising is how many women don’t realize estradiol isn’t just for menopause. It’s also used to treat premature ovarian failure, certain types of infertility, and even severe osteoporosis in younger women. And while most focus on the symptoms, the real value lies in long-term protection — lower fracture rates, better skin elasticity, and even improved sleep quality. But it’s not a one-size-fits-all fix. Genetics, weight, liver health, and even smoking can change how your body responds.
Below, you’ll find real patient stories and practical guides that cover everything from how to tell if your estradiol dose is right, to what happens when you stop it cold turkey, to how it interacts with other common medications like NSAIDs, anticoagulants, and even antibiotics. These aren’t theory pieces — they’re written by people who’ve been there, and they’ll help you make smarter choices without the fluff.
Compare Estrace (Estradiol) with Alternatives: What Works Best for You
Estrace (estradiol) helps with menopause symptoms, but it's not the only option. Compare tablets, patches, vaginal treatments, and non-hormonal alternatives to find what works best for your body and lifestyle.