Disulfiram – How It Works and What You Need to Know
When working with Disulfiram, Disulfiram is a medication that creates a severe reaction if alcohol is consumed. Also known as Antabuse, it helps people with alcohol dependence stay sober by blocking the enzyme aldehyde dehydrogenase. This inhibition is a core part of medication‑assisted treatment for alcohol use disorder.
The key to Disulfiram’s effect lies in its impact on aldehyde dehydrogenase. By stopping this enzyme, the drug lets acetaldehyde – a toxic by‑product of alcohol metabolism – build up in the bloodstream. The result is a rapid onset of flushing, nausea, pounding heart, and headache, which most users find intolerable. In simple terms, Disulfiram creates a powerful aversion: the brain learns to link drinking with immediate, unpleasant sensations, reinforcing abstinence.
Before starting Disulfiram, a patient must be completely alcohol‑free for at least 12 hours, and ideally 24–48 hours, to avoid a dangerous reaction. Doctors usually begin with a low dose, such as 250 mg daily, and may adjust based on liver function tests and how well the person tolerates side effects. Regular monitoring of liver enzymes is essential because the drug can stress the liver, especially in people with pre‑existing liver disease. Compliance is also critical; missing doses reduces its protective effect, while accidental alcohol exposure can be severe.
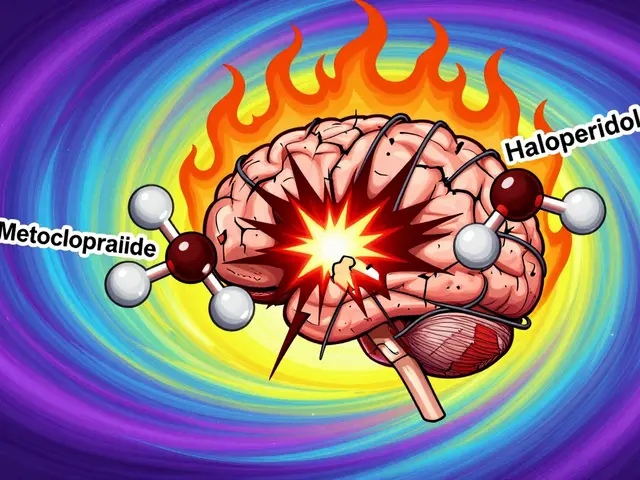
Like any medication, Disulfiram comes with a list of side effects and contraindications. Common complaints include tiredness, skin rash, and a metallic taste. More serious concerns involve liver toxicity, neuropathy, and rare cases of severe psychiatric reactions. It also interacts badly with several drugs, such as metronidazole, certain cephalosporins, and warfarin, so a full medication review is a must before prescribing. Patients should also watch out for hidden sources of alcohol in cough syrups, mouthwashes, and even some foods.
Disulfiram isn’t the only option for alcohol aversion. Naltrexone works by blocking the brain’s pleasure receptors for alcohol, while acamprosate helps restore the balance of neurotransmitters after prolonged drinking. Compared to those, Disulfiram’s approach is more direct and often more noticeable, making it a good fit for people who need a strong deterrent. However, it requires strict adherence and a commitment to avoid any alcohol‑containing products, whereas naltrexone and acamprosate can be taken even if a slip occurs.
Practical tips can make Disulfiram safer and more effective. First, keep a list of all over‑the‑counter products that contain alcohol and share it with family members. Second, use a medication‑reminder app to maintain daily dosing. Third, pair the drug with behavioral counseling or support groups; the combination of a pharmacological deterrent and psychosocial support yields the best long‑term outcomes. Finally, if any unusual symptoms appear – especially severe nausea, chest pain, or yellowing of the skin – seek medical help immediately.
Key Takeaways for Using Disulfiram Safely
Disulfiram blocks aldehyde dehydrogenase, causing acetaldehyde buildup and a rapid aversive reaction to alcohol. It is most effective when part of a broader medication‑assisted treatment plan that includes counseling and regular liver monitoring. Understanding drug interactions, hidden alcohol sources, and the importance of strict adherence can prevent dangerous side effects and boost the chance of lasting sobriety.
Below you’ll find a curated list of articles that dive deeper into Disulfiram’s mechanisms, compare it with other alcohol‑use medications, and offer real‑world tips for staying safe while on therapy. Explore the collection to get the full picture and make an informed decision about whether Disulfiram fits your recovery journey.
Acamprosate vs Alternatives: Efficacy, Safety, and Choosing the Right Treatment
A detailed comparison of Acamprosate with naltrexone, disulfiram, baclofen and topiramate, covering efficacy, safety, dosing and how to pick the right AUD medication.