Rifampin Interaction Calculator
Estimate Your Required Dosage Adjustment
Rifampin significantly reduces levels of anticoagulants and antivirals. This tool provides estimated dosage adjustments based on documented interaction studies.
Enter your drug type and baseline dose to see estimated adjustment
When you’re on rifampin for tuberculosis or to prevent meningitis, you might not think twice about other meds you’re taking. But if you’re also on a blood thinner or an antiviral, this one antibiotic could be quietly sabotaging your treatment. Rifampin doesn’t just kill bacteria-it triggers your liver to speed up the breakdown of many other drugs, often dropping their levels by more than half. This isn’t a theoretical risk. It’s a real, documented danger that’s sent people to the hospital with clots, strokes, or failed viral control.
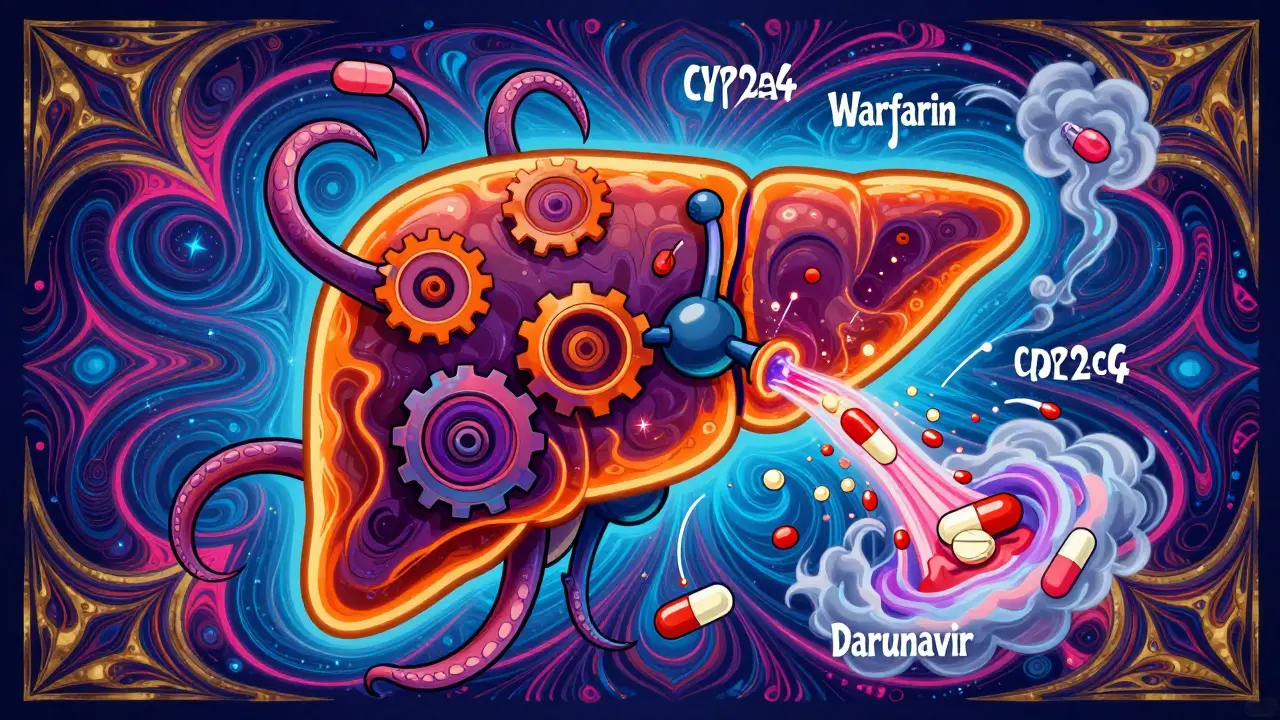
How Rifampin Changes Your Body’s Drug Processing
Rifampin doesn’t block enzymes. It flips a switch. It activates something called the pregnane X receptor (PXR), a master regulator in your liver and gut. Once activated, PXR tells your body to make more of certain enzymes-especially CYP3A4 and CYP2C9-and to pump out more of a protein called P-glycoprotein. These aren’t just random proteins. They’re the main tools your body uses to break down and remove drugs from your system.
Think of it like turning up the speed on a factory assembly line. Your liver starts churning out drug-metabolizing enzymes faster than normal. The result? Drugs that used to stick around for hours now get cleared in minutes. The effect starts within 24 to 48 hours of starting rifampin. By day five or seven, it’s at full force. And here’s the kicker: even after you stop rifampin, it takes two to three weeks for your liver to calm down and return to normal. That means the interaction doesn’t end when the antibiotic does.
Anticoagulants: When Blood Thinners Become Too Weak
If you’re on warfarin, the classic vitamin K antagonist, rifampin can slash its effectiveness by up to 74%. That’s not a small drop. It’s enough to turn a therapeutic INR of 2.5 into a dangerous 1.2-putting you at serious risk of clots. One case report described a woman with a mechanical heart valve whose INR dropped to normal levels after adding rifampin. She didn’t feel sick. No symptoms. But she was on the edge of a stroke or pulmonary embolism. Her doctors had to switch her to injectable heparin until rifampin was fully cleared.
It’s not just warfarin. The newer direct oral anticoagulants (DOACs)-dabigatran, apixaban, rivaroxaban, edoxaban-are just as vulnerable. Studies show rifampin cuts dabigatran and apixaban levels by 50-67%. Rivaroxaban drops by about 60%. Even edoxaban, which seems a little more stable, still sees a 35% reduction. And here’s the problem: unlike warfarin, you can’t easily check if these drugs are working. There’s no routine blood test. You’re flying blind.
That’s why guidelines from the European Heart Rhythm Association and the American College of Chest Physicians say the same thing: avoid combining rifampin with DOACs if you can. If you absolutely can’t, you need to switch to something else-like low molecular weight heparin injections-during the course of rifampin treatment. And even then, you need to monitor closely.
Antivirals: The Hidden Risk in HIV and Hepatitis Treatment
The same problem hits antivirals hard. Many HIV medications-especially protease inhibitors like darunavir and atazanavir-are broken down by CYP3A4. When rifampin is added, their levels can plunge by 80% or more. That’s not just a drop in effectiveness. It’s a recipe for treatment failure and drug resistance. A single missed dose of antiviral can allow the virus to mutate and become untreatable. That’s why combining rifampin with most HIV drugs is considered a contraindication.
Hepatitis C treatments are no better. Drugs like elbasvir/grazoprevir and sofosbuvir/velpatasvir are also metabolized by CYP3A4. Rifampin can cut their concentrations so low that the cure rate drops from over 95% to near zero. For someone with chronic hepatitis, that means months of treatment wasted-and the disease still there.
Some antivirals, like tenofovir or lamivudine, aren’t affected as much because they don’t rely on CYP enzymes. But the ones that do? They’re off-limits with rifampin. And if you’re on both, your doctor needs to know-before you start.

What Do Doctors Actually Do When This Happens?
In real-world practice, things get messy. A 2023 study of over 2,000 patients found that while guidelines say to avoid rifampin with DOACs, 15% of patients still get both. Why? Because sometimes there’s no choice. A patient with tuberculosis and atrial fibrillation might not tolerate heparin injections. Or maybe they’re in a rural area without easy access to daily injections.
So what do doctors do? They try to manage it. For warfarin users, they often bump the dose by three to five times. Some use point-of-care INR monitors-devices you can use at home-to check levels every few days. But even then, it’s risky. One wrong dose, one missed test, and you’re in trouble.
For DOACs, the options are even scarcer. Only 12% of U.S. hospitals have formal protocols for handling rifampin-DOAC interactions. Most rely on guesswork. Some try doubling the DOAC dose. But that’s not backed by solid data. It’s a gamble. And if the rifampin stops, the drug levels can spike dangerously high, leading to bleeding.
One study on rivaroxaban suggested a slow, stepwise adjustment-gradually increasing the dose while rifampin is active, then tapering it back down after stopping. But that’s not standard practice. It’s still experimental.
What’s Being Done to Fix This?
The pharmaceutical industry knows this is a huge problem. That’s why new anticoagulants are being designed to avoid CYP metabolism entirely. Milvexian, a factor XIa inhibitor now in late-stage trials, is one example. Early data suggest it’s not affected by rifampin or other strong enzyme inducers. That’s a game-changer. If approved, it could be the first anticoagulant you can safely use with rifampin.
The FDA now requires all new drugs to be tested against strong inducers like rifampin before approval. That means newer medications-especially antivirals and anticoagulants-are being labeled with clearer warnings. But the problem isn’t going away. Rifampin is still the go-to drug for tuberculosis in many parts of the world. And tuberculosis doesn’t wait for perfect drug combinations.

What Should You Do If You’re on Rifampin?
If you’re prescribed rifampin, here’s what you need to do right now:
- Tell your doctor every medication you’re taking-even over-the-counter pills, supplements, or herbal products. Many people forget that St. John’s wort also induces CYP3A4 and makes this worse.
- Ask: Is there an alternative to rifampin? For tuberculosis, sometimes other antibiotics like rifabutin can be used instead. Rifabutin is a weaker inducer and might be safer with your other meds.
- If you’re on a blood thinner, ask whether switching to heparin is possible. Even if it means daily shots, it’s safer than risking a clot.
- If you’re on an antiviral, don’t stop or change your dose on your own. Talk to your infectious disease specialist. They may need to switch your antiviral or adjust the timing.
- Don’t assume it’s safe after you stop rifampin. Wait at least two weeks before restarting your anticoagulant or antiviral without medical supervision.
This isn’t just about following rules. It’s about survival. A single interaction can turn a treatable condition into a life-threatening emergency. And the worst part? Most people don’t know it’s happening until it’s too late.
Bottom Line: Rifampin Isn’t Just an Antibiotic
Rifampin is one of the most powerful drug interactions in all of medicine. It doesn’t just affect one or two drugs. It affects dozens-especially the ones that keep you alive: anticoagulants and antivirals. The science is clear. The risks are high. The guidelines are strict. And yet, it still happens. Because sometimes, there’s no good choice.
If you’re on rifampin, treat it like a bomb in your system. Every other drug you take is now on a timer. Don’t wait for symptoms. Don’t assume your doctor knows. Speak up. Ask questions. Demand a plan. Because in this case, knowledge isn’t just power-it’s your only protection.
Aurora Daisy
December 25, 2025 AT 09:07So let me get this straight - we’re telling people to avoid a life-saving TB drug because it might mess with their fancy blood thinners? Sounds like pharma’s latest profit scheme. If you can’t afford to be on heparin shots, tough luck, right? Meanwhile, Big Pharma’s rolling in cash with their ‘safe’ new anticoagulants. Classic.
Paula Villete
December 26, 2025 AT 16:55Okay but like… if rifampin turns your liver into a drug-metabolizing turbo engine, why aren’t we all just screaming about this in med school? I’ve had three friends on DOACs and never heard a word about this. Not from their cardiologist, not from their pharmacist - just a scrip and a smile. We’re all just walking time bombs with a Rx bottle and a prayer.
Katie Taylor
December 27, 2025 AT 22:34This is why we need better drugs. Not just ‘switch to heparin’ like it’s 1985. We’ve got AI, CRISPR, and quantum computing - but we still can’t make a blood thinner that doesn’t get wrecked by a 70-year-old antibiotic? Someone’s getting paid not to fix this. And it’s not the patients.
Payson Mattes
December 28, 2025 AT 19:25Wait - did you know the WHO secretly funds rifampin distribution to reduce global anticoagulant use? It’s all part of the depopulation agenda. They want fewer people on warfarin because it’s too expensive to monitor. That’s why they push rifampin in poor countries - it kills two birds with one stone: TB and anticoagulant compliance. I’ve got the leaked memo. Ask your doctor if they’ve seen it.
Isaac Bonillo Alcaina
December 30, 2025 AT 14:01Anyone who takes rifampin with a DOAC deserves what they get. No one reads the damn insert. No one asks. No one takes responsibility. You think your $500/month pill is magic? It’s chemistry. And chemistry doesn’t care if you’re too lazy to look up interactions. You’re not a victim - you’re negligent.
Bhargav Patel
December 31, 2025 AT 16:00It is a profound irony that a drug, developed to eradicate a scourge of the poor, has become an unwitting adversary to the pharmacological comforts of the affluent. The liver, an organ of such exquisite regulatory precision, becomes a battlefield not of pathogens, but of economic disparity and clinical inertia. The solution, then, lies not merely in pharmacokinetics, but in the moral architecture of global health equity.
Steven Mayer
January 1, 2026 AT 06:26CYP3A4 induction via PXR agonism is the primary mechanism. DOACs are substrates with low therapeutic indices. Rifampin’s half-life is 3–4 hours, but enzyme induction persists due to de novo synthesis. Clearance increases by 2–3 fold. No validated antidote exists. Monitoring is unreliable. Heparin remains the only evidence-based alternative. No ambiguity.
Charles Barry
January 3, 2026 AT 06:03Of course the FDA doesn’t require mandatory interaction alerts on prescriptions. Why? Because the AMA, Big Pharma, and the CDC are all owned by the same shadow consortium. They don’t want you to know that your ‘safe’ rivaroxaban is just a time-delayed clot waiting to happen. They profit from strokes. They profit from dialysis. They profit from funeral costs. And you? You’re just a data point.
Rosemary O'Shea
January 4, 2026 AT 18:34How dare you reduce this to a mere pharmacokinetic interaction? This is a tragedy of modern medicine - where we optimize for convenience over consequence. We give people a pill for everything, then act shocked when the system collapses under its own weight. Rifampin isn’t the villain - our arrogance is. We treat biology like a software update. It’s not. It’s a symphony. And we’re deaf.
Bartholomew Henry Allen
January 5, 2026 AT 01:41