Sodium Imbalance: Causes, Symptoms, and How It Affects Your Health
When your body’s sodium imbalance, a condition where blood sodium levels fall outside the normal range of 135–145 mEq/L. Also known as electrolyte imbalance, it can be life-threatening if ignored. Sodium isn’t just table salt—it’s the main electrolyte that controls fluid balance, nerve signals, and muscle function. Too little (hyponatremia, a condition where sodium drops below 135 mEq/L, often from overhydration, heart failure, or certain medications) or too much (hypernatremia, a condition where sodium rises above 145 mEq/L, usually from dehydration or kidney problems) throws your whole system off. It’s not rare—up to 30% of hospitalized patients show signs of it, and many don’t even know why they feel off.
What causes sodium imbalance? It’s rarely just one thing. Drinking too much water after a marathon can dilute your sodium. Diuretics, antidepressants, or thyroid issues can mess with how your kidneys hold onto sodium. Chronic kidney disease, like the kind discussed in posts about edema in CKD, fluid retention caused by poor sodium control and impaired kidney filtering, directly links to sodium problems. Even simple things like skipping meals or eating too much processed food can nudge your levels out of range. The body tries to fix itself, but when the kidneys are damaged or hormones like ADH go haywire, it can’t keep up.
Symptoms are easy to miss. You might think you’re just tired, dizzy, or got a headache. But if you’re confused, nauseous, or have muscle cramps without a clear reason, sodium could be the culprit. Severe cases lead to seizures, coma, or brain swelling. The good news? Most mild imbalances can be fixed with small changes—cutting back on water if you’re overhydrating, adjusting meds, or eating more sodium-rich foods if you’re low. But it’s not something to guess at. If you’re on diuretics, have kidney disease, or take meds like SGLT2 inhibitors (which pull sodium out through urine), you’re at higher risk.
The posts below dig into real cases and connections. You’ll find how diuretics and salt restriction work together in kidney disease, how certain drugs like rifampin or amlodipine can indirectly affect sodium, and why talking to your pharmacist about supplements and food interactions matters. This isn’t just about numbers on a lab report—it’s about how your daily habits, medications, and health conditions all tie into your body’s sodium balance. What you read here could help you spot a problem before it becomes serious.
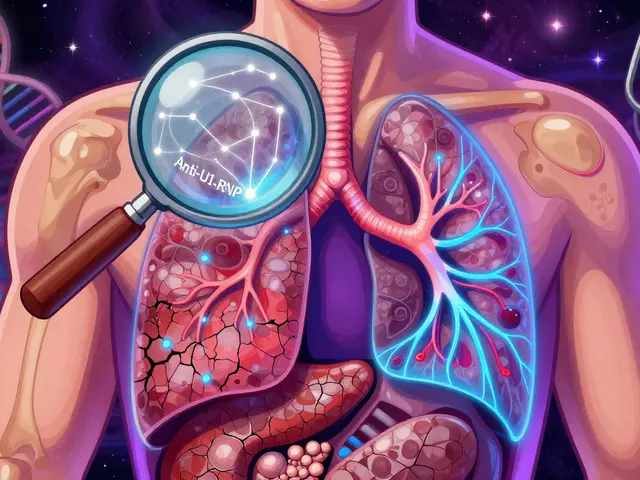
Hyponatremia and Hypernatremia in Kidney Disease: What You Need to Know
Hyponatremia and hypernatremia are dangerous sodium imbalances common in kidney disease. Learn how reduced kidney function causes them, why standard treatments can backfire, and what actually works to stay safe.