When your kidneys start to fail, they don’t just stop filtering waste. They also lose their ability to keep your sodium levels in check. That’s when things get dangerous. Hyponatremia (low sodium) and hypernatremia (high sodium) aren’t just lab values-they’re life-threatening conditions that hit hard in people with chronic kidney disease (CKD). Around 1 in 5 people with advanced CKD will develop one of these sodium disorders, and many don’t even know it until they’re in the hospital.
Why Your Kidneys Control Your Sodium
Your kidneys are like precision engineers for your body’s fluid balance. Every day, they filter about 180 liters of blood. They reabsorb what you need and flush out the rest. Sodium is one of the main things they manage. When you eat salt, your kidneys decide how much to hold onto and how much to pee out. Water follows sodium. So if sodium goes up, your body holds more water. If sodium drops, you lose water. In healthy people, this system works smoothly. But in CKD, the filters break down. By stage 4 or 5 (when GFR drops below 30 mL/min), your kidneys can’t make concentrated urine anymore. That means they can’t hold onto water when you’re dehydrated, and they can’t flush out extra water when you drink too much. The result? Sodium levels swing out of control.Hyponatremia: When Sodium Drops Too Low
Hyponatremia is defined as a serum sodium level below 135 mmol/L. In CKD, it’s the most common sodium disorder-making up 60-65% of cases. The biggest reason? Your kidneys can’t get rid of excess water. Think of it this way: You drink a glass of water. A healthy kidney says, “Okay, I’ll pee that out.” A kidney with advanced CKD says, “I don’t know how to do that anymore.” So the water stays in your blood, diluting the sodium. It’s not that you’re low on sodium-it’s that you have too much water. Common triggers include:- Drinking too much water, especially if you’re elderly or have reduced thirst awareness
- Using thiazide diuretics (like hydrochlorothiazide), which are less effective in CKD but still used
- Too much protein, potassium, or sodium restriction-yes, even “healthy” diets can backfire
- Medications like SSRIs, NSAIDs, or certain blood pressure drugs that affect ADH (vasopressin)
Hypernatremia: When Sodium Gets Too High
Hypernatremia means your sodium level is above 145 mmol/L. It’s less common than hyponatremia in CKD, but just as dangerous. This happens when you lose too much water-or don’t drink enough. In advanced CKD, people often don’t feel thirsty. They might be on fluid restrictions because of swelling or heart failure. If they’re also sweating, vomiting, or on diuretics, they can become dehydrated fast. Their kidneys can’t concentrate urine to save water, so they keep losing it. Elderly patients are especially at risk. A 75-year-old with CKD who doesn’t drink because they’re afraid of swelling can slip into hypernatremia without realizing it. Symptoms include extreme thirst, dry mouth, confusion, muscle twitching, and seizures. If not corrected slowly, rapid water replacement can cause brain swelling-another life-threatening problem.Three Types of Hyponatremia in CKD
Not all hyponatremia is the same. Doctors classify it by your body’s fluid volume:- Euvolemic (most common): Normal fluid volume, but too much water. This is the classic CKD case-kidneys can’t excrete water.
- Hypovolemic: You’ve lost both water and sodium, but lost more sodium. Think diuretic overuse, salt-wasting kidney disease, or vomiting.
- Hypervolemic: You have too much total body water and sodium. This happens with severe edema, heart failure, or nephrotic syndrome.

What Happens If You Correct Sodium Too Fast?
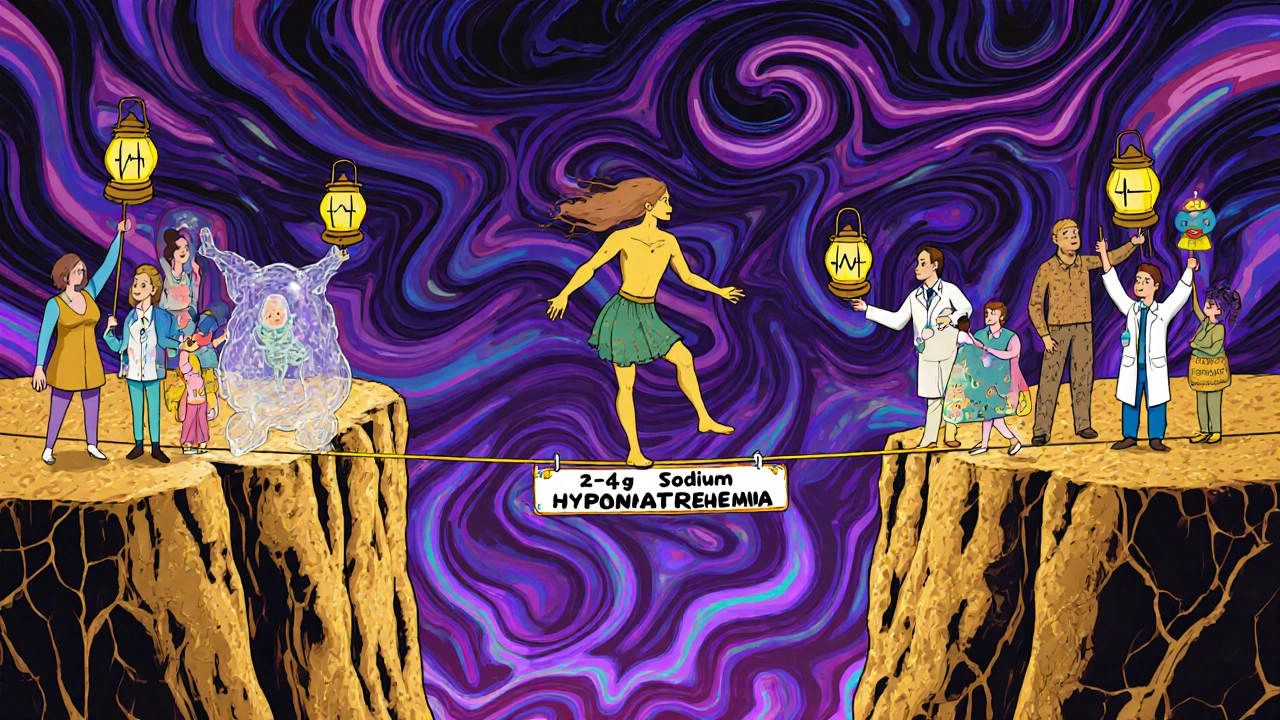
One of the biggest mistakes doctors make is rushing to fix sodium levels. The rule in CKD is simple: Go slow. Raising sodium by more than 8 mmol/L in 24 hours can cause osmotic demyelination syndrome (ODS). This is when brain cells shrink and die because the body can’t adjust to the sudden change. ODS doesn’t always show up right away-it can take days. Patients might seem fine after correction, then suddenly develop paralysis, trouble swallowing, or locked-in syndrome. In CKD patients, the risk is even higher because their brains have been exposed to low sodium for longer. Studies show 12-15% of ODS cases in CKD patients happen because standard correction protocols were applied without adjusting for kidney function. The safe target? No more than 4-6 mmol/L in the first 24 hours. For mild cases, sometimes just stopping water intake is enough.Fluid and Salt: The Tightrope Walk
Dietary advice for CKD is confusing. You’re told to cut salt to control blood pressure. You’re told to limit fluids to reduce swelling. You’re told to cut protein to protect your kidneys. But cutting all three can make hyponatremia worse. Why? Because your kidneys need solutes-sodium, potassium, protein-to make urine. If you eat too little, your kidneys can’t excrete water. They’re like a factory with no raw materials. The result? Water builds up. Sodium gets diluted. Experts now warn against extreme restrictions. In advanced CKD, a daily sodium intake of 2-4 grams is often safer than 1 gram. Fluid intake should be individualized: 1,000-1,500 mL/day for early CKD, 800-1,000 mL/day for stage 4-5. A 2020 study found that patients who got three or more sessions with a renal dietitian were far less likely to end up in the hospital for sodium problems. Understanding what “low sodium” really means matters.Medications That Make It Worse
Some drugs are okay for healthy people but risky in CKD:- Thiazide diuretics: These are common for high blood pressure, but they stop working when GFR drops below 30. Worse-they increase hyponatremia risk. The FDA warns against using them in advanced CKD.
- Vaptans (like tolvaptan): These block vasopressin and help flush water. Great for liver disease. But in CKD, the kidneys can’t respond. They’re ineffective and can cause liver damage. The EMA bans them in stage 4-5 CKD.
- SSRIs and NSAIDs: These can trigger inappropriate ADH release. If you’re on these and have CKD, monitor sodium every 3-6 months.
New Tools for Better Management
There’s hope. In March 2023, the FDA approved a new sodium monitoring patch for CKD patients. It measures sodium levels in the skin every few hours and syncs with an app. In trials, it matched blood tests 85% of the time. No more waiting for lab results. The 2024 KDIGO guidelines are expected to recommend personalized fluid targets based on your residual kidney function-not a one-size-fits-all number. This could change how we treat sodium disorders forever.What You Can Do
If you have CKD, here’s what works:- Don’t guess your fluid intake. Ask your nephrologist or dietitian for your daily limit.
- Don’t cut salt to zero. 2-4 grams per day is often safe. Use herbs, lemon, or vinegar for flavor.
- Watch for symptoms: confusion, nausea, dizziness, weakness, falls.
- Get your sodium checked every 3-6 months-even if you feel fine.
- Review all your meds with your pharmacist. Many common drugs can cause or worsen sodium imbalance.
- If you’re on a fluid restriction, keep a daily log. Write down everything you drink, including soup, ice, yogurt.
When to Call Your Doctor
Call immediately if you have:- Sudden confusion or memory loss
- Severe nausea or vomiting
- Loss of balance or frequent falls
- Seizures or muscle twitching
- Extreme thirst with dry mouth (possible hypernatremia)
Mark Kahn
November 21, 2025 AT 21:38Just wanted to say this post saved my life. My dad has stage 4 CKD and we were clueless about sodium until we read this. Now we’re tracking his fluids like a science experiment-no more guessing. Thanks for breaking it down so clearly.
Leo Tamisch
November 23, 2025 AT 00:18How quaint. You treat sodium as if it’s a mystical force governed by divine renal algorithms. In truth, it’s just osmotic physics-reducible to entropy and ion gradients. The real tragedy? We’ve anthropomorphized kidneys into ‘guardians’ when they’re merely biological pumps with failing firmware.
Still… the patch is a nice touch. At least we’re moving from medieval blood draws to wearable telemetry. Progress, albeit slow.
Clifford Temple
November 23, 2025 AT 21:17Why are we letting foreign medical guidelines dictate how we treat Americans? The KDIGO guidelines? That’s a European committee with no clue about real US kidney patients. We need American-made solutions-not some WHO-approved water rationing plan.
And who approved this ‘2-4 grams sodium’ nonsense? That’s just feeding the system. We need STRONGER restrictions, not more leniency. This is weak.
Corra Hathaway
November 25, 2025 AT 12:09Okay but can we talk about how wild it is that we’ve been treating kidneys like broken coffee machines for decades? 🤯
One minute you’re told to drink less, next you’re told to eat more salt, then someone says ‘don’t take your meds’… it’s like medical whack-a-mole. But THIS? This post is the cheat code. 💪
Also, I’m telling my entire family. No more ‘just drink water’ advice. Ever.
Shawn Sakura
November 26, 2025 AT 12:13Ths is amazin. I had no idea tht thiazide diuretics could be so dangours in CKD. My doc still prescribes them and I’ve been feeling weird lately. Gonna make an appt ASAP. Thank you for the info, even with my typos. 😊
Paula Jane Butterfield
November 27, 2025 AT 13:32As a renal dietitian, I see this every day. Patients panic about salt and end up drinking 3 liters of water a day because they think ‘water is good.’ Meanwhile, their sodium plummets.
Education is everything. We need more of these posts-not just from doctors, but from patients who’ve been there. I’ve started handing out printed versions in clinic. If you’re reading this and have CKD: don’t be afraid to ask your team for a sodium check. It’s a simple blood test. It could save your brain.
Simone Wood
November 29, 2025 AT 02:48I’ve been monitoring my sodium for 8 years now and I can tell you-this is all just a pharmaceutical ploy. The patch? A scam. The ‘2-4 grams’ advice? Designed to keep you buying electrolyte drinks and ‘renal-friendly’ branded salt substitutes. The real cause of hyponatremia in CKD? Glyphosate in the water supply. They don’t want you to know that.
My cousin’s nephrologist got fired for saying this. Now he’s in hiding. #WatchYourWater
Swati Jain
November 30, 2025 AT 11:18Wow. So you’re telling me that in India, where people drink 3 liters of water daily with zero sodium intake, we’re basically doing a slow-motion suicide experiment? 😅
My aunt had CKD and drank coconut water like it was holy water. Now she’s on dialysis. This post is 100% accurate. We need to stop treating ‘hydration’ like a virtue. It’s a medical variable. Not a yoga pose.
Florian Moser
December 1, 2025 AT 13:06This is one of the most well-researched, clearly articulated summaries on sodium management in CKD I’ve ever encountered. The breakdown of euvolemic/hypovolemic/hypervolemic hyponatremia alone is worth a medical textbook chapter. Thank you for emphasizing the slow correction protocol-this is the single most overlooked danger in clinical practice. I’ve shared this with my entire nephrology team.
jim cerqua
December 3, 2025 AT 03:45THEY’RE KILLING US WITH GOOD INTENTIONS. 🚨
Let me tell you what happens when you tell a 72-year-old man to ‘drink less water’ because he’s got CKD… he stops drinking. Then he gets hypernatremia. Then he has a seizure. Then they rush him in. Then they give him 3 liters of IV fluid in 4 hours. Then he dies of osmotic demyelination.
It’s not a disease. It’s a SYSTEMIC FAILURE. Every single doctor who rushes correction needs to be held accountable. Every dietitian who says ‘no salt’ without context is a liability. This isn’t medicine. It’s a death sentence wrapped in a pamphlet.
Donald Frantz
December 3, 2025 AT 16:34Interesting. The data on ODS risk in CKD patients is compelling, but I’m curious about the sample sizes in those studies. Most are single-center with under 200 patients. Are we extrapolating too broadly? Also, how does residual renal function correlate with correction safety thresholds? I’d love to see the raw data behind the 4-6 mmol/L guideline.
Julia Strothers
December 4, 2025 AT 13:15So let me get this straight-FDA approved a skin patch that ‘matches blood tests 85% of the time’? That’s not a medical device, that’s a beta test. And they’re letting patients use it? What’s next? A TikTok app that diagnoses hyponatremia from your selfie?
And why is no one talking about how the ‘2-4g sodium’ advice is just Big Pharma’s way to sell ‘renal salts’? I’ve seen the patents. This is all connected. The guidelines, the patch, the dietitians-it’s a money pipeline. You’re being played.
Mark Kahn
December 5, 2025 AT 17:11Hey @Florian Moser - you’re right. The 4-6 mmol/L rule is everything. My dad’s doctor almost pushed him to +10 in 24 hours last year. We had to push back hard. I’m glad someone else is saying this out loud.