Chronic Kidney Disease: Causes, Management, and What You Need to Know
When your chronic kidney disease, a long-term condition where kidneys lose their ability to filter waste and excess fluid from the blood. Also known as CKD, it often creeps up without symptoms until damage is advanced. It’s not just about reduced urine output—it’s about your whole body struggling to stay balanced. Blood pressure spikes, toxins build up, and your bones, heart, and nerves start paying the price. Around 1 in 7 adults in the U.S. has some level of CKD, and most don’t know it until a routine blood test reveals it.
What makes CKD tricky is how it connects to other conditions. For example, SGLT2 inhibitors, a class of diabetes drugs like Jardiance and Farxiga that help the kidneys remove sugar through urine are now used not just for blood sugar control, but specifically to slow kidney decline—even in people without diabetes. These drugs don’t just lower glucose; they reduce pressure inside the kidney’s filtering units, cutting inflammation and scarring. Then there’s edema in CKD, the swelling in legs, ankles, or hands caused by fluid buildup because kidneys can’t remove sodium properly. This isn’t just discomfort—it’s a warning sign your body’s fluid balance is failing. Doctors tackle it with a mix of diuretics for kidney disease, medications that help the body flush out extra water, strict salt limits, and even compression socks. No single fix works alone; it’s the combo that matters.
People with CKD often take multiple medications—some for blood pressure, others for anemia or bone health. But drugs like certain antibiotics or painkillers can make kidney damage worse. That’s why talking to your pharmacist about every pill, supplement, or herb you take is non-negotiable. You’re not just managing symptoms—you’re protecting what’s left of your kidney function. The good news? Early detection and smart lifestyle changes can delay or even prevent dialysis. It’s not about perfection; it’s about consistency—watching your salt, staying active, controlling blood sugar and pressure, and getting regular check-ups.
Below, you’ll find real, practical guides on how these pieces fit together: how SGLT2 inhibitors protect your kidneys, why diuretics work the way they do, how to handle swelling without overdoing it, and what to ask your doctor when your meds don’t seem to be helping. No fluff. Just what works.
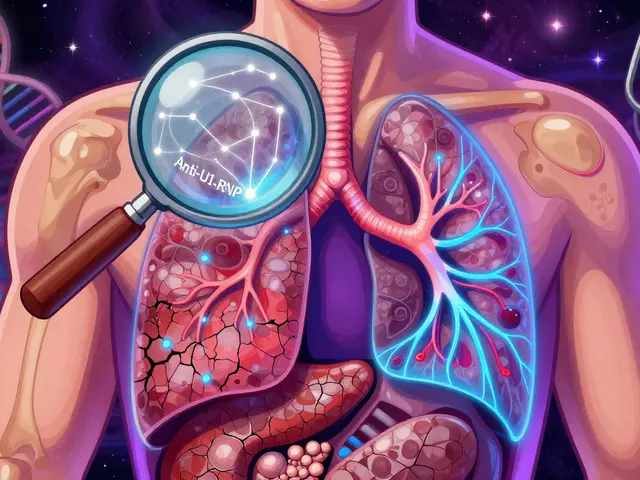
Hyponatremia and Hypernatremia in Kidney Disease: What You Need to Know
Hyponatremia and hypernatremia are dangerous sodium imbalances common in kidney disease. Learn how reduced kidney function causes them, why standard treatments can backfire, and what actually works to stay safe.