Every year, millions of people miss doses of their medications-not because they don’t care, but because the system is working against them. A medication adherence rate of just 50% is the norm for chronic conditions like high blood pressure, diabetes, and heart disease. That means half the people taking pills for life-threatening illnesses aren’t taking them right. And it’s not laziness. It’s a mix of real, everyday problems that no one talks about enough.
Forgetting Is the Biggest Problem-And It’s Not Your Fault
Think about your own week. Work runs late. Kids get sick. You travel. Your phone dies. Suddenly, you’re not sure if you took your pill this morning-or if you took it yesterday. This isn’t carelessness. It’s human.
Studies show that 44% of diabetic patients over 59 say forgetfulness is their main barrier. That’s nearly half. For people taking multiple medications, it gets worse. Imagine six different pills at three different times of day. Even with alarms, your brain gets overloaded. A 2023 meta-analysis of 74 studies found that adherence drops from 79% for once-daily meds to just 51% for four or more doses per day. The more times you have to remember, the more likely you are to mess up.
Cost Keeps People From Even Starting
It’s not just about forgetting. Sometimes, people never fill the prescription at all. The CDC reports that 20% to 30% of new prescriptions are left at the pharmacy because of cost. A $50 co-pay for a monthly medication? That’s a meal. A $300 insulin pen? That’s rent.
One in two patients says cost is a primary reason they skip doses or cut pills in half. This isn’t just about being uninsured. Even people with insurance skip meds because their plan has high deductibles or the drug isn’t on the formulary. A 2023 AMA survey found that 50% of patients cite cost as the top barrier. And it’s not just insulin-blood pressure pills, cholesterol meds, even antidepressants get skipped when budgets are tight.
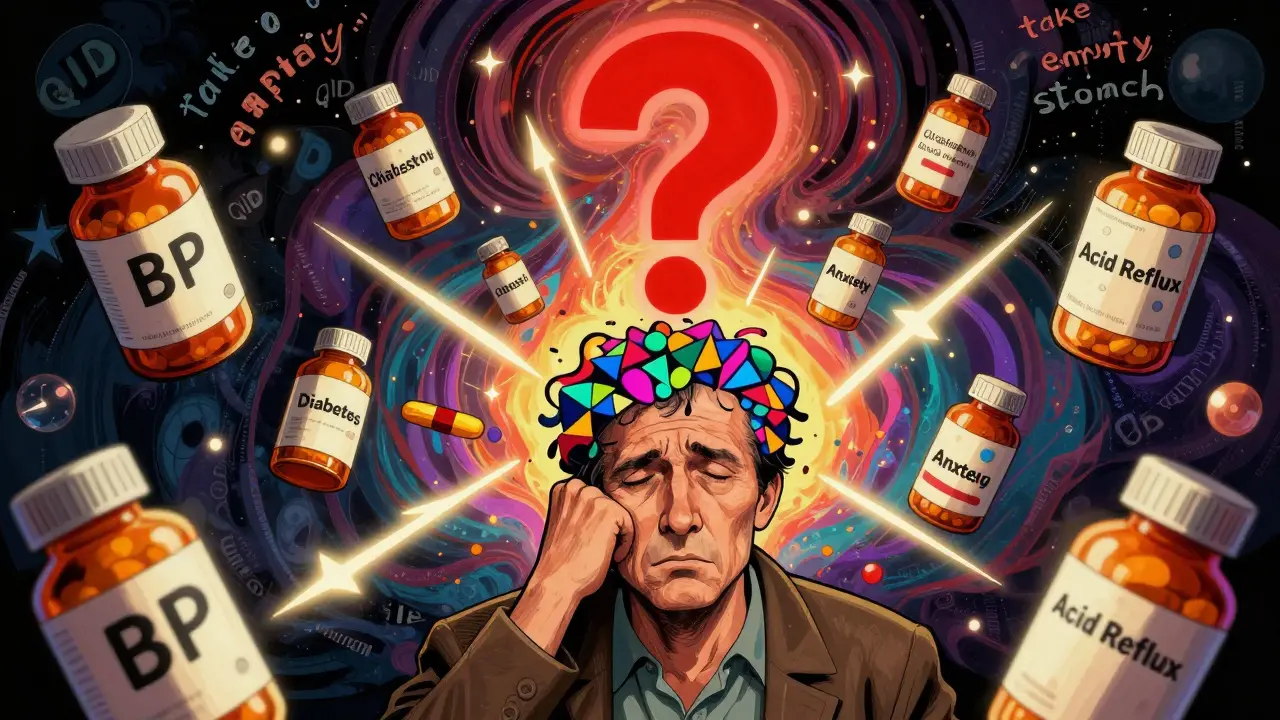
Too Many Pills, Too Many Rules
Polypharmacy-taking five or more medications-is common for older adults and people with chronic conditions. But each extra pill increases your chance of nonadherence by 16%. That’s not a small number. It’s a mathematical trap.
Imagine this: one pill for blood pressure, two for diabetes, one for arthritis, one for anxiety, and another for acid reflux. Each has different instructions: take with food, take on empty stomach, take at night, take in the morning, don’t lie down after. Some need to be spaced 12 hours apart. Some can’t be taken with grapefruit. You’re not a pharmacist. You’re just trying to survive.
Doctors often prescribe these without realizing how overwhelming they are. A patient on Reddit shared: “I have five meds. Three have different times. I miss at least two doses a week because my job shifts change.” That’s not laziness. That’s a system that doesn’t work for real life.

Confusing Instructions and Poor Communication
Ever tried reading the tiny print on an insulin pen? Or followed instructions written in medical jargon like “take QID” (four times a day)? Many patients can’t read them. A 2024 study found that 40% of diabetic patients over 59 said poor health literacy was a barrier.
And it’s not just about reading. It’s about understanding. One patient on HealthUnlocked said: “My doctor never told me why I had to take my blood pressure pill at night. I switched it to morning because that’s when I remembered. My readings got worse.” That’s not the patient’s fault. That’s a failure in communication.
Eighty-four percent of diabetic patients said they didn’t get enough guidance when starting a new med. Most doctors have 15 minutes per visit. They’re rushing. Patients leave confused. And confusion leads to skipping.
Side Effects Scare People Away
People don’t skip meds because they’re rebellious. They skip them because they’re scared.
Thirty-eight percent of nonadherence cases come from fear of side effects. A patient on Drugs.com wrote: “My cholesterol pill gave me muscle pain. I didn’t know it was normal. I thought I was damaging my heart. I stopped.”
Doctors often don’t talk about side effects unless asked. And patients rarely ask. They assume the side effect is permanent, or worse-that it means the drug is harming them. But many side effects fade after a few weeks. Without explanation, people assume the risk outweighs the benefit.
Even worse: some patients feel guilty for taking meds they don’t understand. They think, “If I really cared about my health, I’d take it.” That guilt doesn’t help. It makes them feel broken.
Life Gets in the Way
It’s not just about the pill. It’s about your life.
Patients with unstable housing, no transportation, or no phone can’t refill prescriptions. A 2023 Robert Wood Johnson Foundation report found that patients in “pharmacy deserts”-areas without nearby pharmacies-have 37% higher nonadherence rates. If you don’t have a car, and the nearest pharmacy is 20 miles away, you’re not going.
People working two jobs, caring for aging parents, or managing mental illness don’t have the mental bandwidth to manage a complex medication schedule. A 2022 survey found that 78% of nonadherent patients struggled with remembering timing. That’s not a memory issue. It’s a life issue.

What Actually Works to Fix This
There’s no magic bullet. But some solutions are proven.
- Simplify the regimen. Switch from three daily pills to one combination pill. Use long-acting versions. Reduce dosing frequency. This alone can boost adherence by 20% or more.
- Automate refills. 90-day mail-order prescriptions increase adherence by 15-20%. No more running out. No more trips to the pharmacy.
- Use pharmacy synchronization. Get all your meds on the same refill date. One trip. One stop. One reminder.
- Train pharmacists to talk. Pharmacists spend more time with patients than doctors. They can explain how to take meds, warn about side effects, and check if cost is an issue. Pharmacies that offer adherence counseling see 18% better adherence.
- Use pill organizers with alarms. Not apps. Not smartwatches. Simple, physical pill boxes with time labels. Many older adults find tech overwhelming. A 2023 University of Michigan study found they need 3-5 sessions just to learn how to use an app.
Here’s the truth: most adherence programs fail because they focus on telling people to “remember.” But the problem isn’t memory. It’s complexity, cost, confusion, and life.
It’s Not About Willpower
Doctors often blame patients. “Why didn’t you take your pills?” But the real question is: “Why did we make it so hard?”
Medication adherence isn’t about discipline. It’s about design. If the system doesn’t work for real people, then the problem isn’t the patient. It’s the system.
Patients aren’t failing. They’re responding to a system that doesn’t respect their time, their money, or their humanity.
Why do so many people skip their medications even when they know it’s important?
People don’t skip meds because they’re careless. They skip because the system is stacked against them. Too many pills, confusing instructions, high costs, side effects, and busy lives make adherence nearly impossible. It’s not about willpower-it’s about design. If taking your medicine requires solving a puzzle every day, most people will give up.
Is forgetting really that big of a problem?
Yes. Forgetfulness is the #1 practical barrier. Studies show 44% of diabetic patients over 59 say they miss doses because they forget. For people on multiple medications, the brain gets overloaded. Even with alarms, shifting schedules, stress, or travel make it easy to lose track. It’s not a memory disorder-it’s a system flaw.
How does cost really affect whether someone takes their medicine?
Cost is the biggest barrier for many. The CDC says 20-30% of prescriptions are never filled because of price. Even with insurance, high copays or deductibles make meds unaffordable. People cut pills in half, skip days, or stop entirely. This isn’t just about being poor-it’s about being priced out of health. A $300 insulin pen isn’t a luxury-it’s a life-or-death choice.
Why do doctors prescribe so many pills if it makes adherence worse?
Doctors often follow guidelines for each condition separately. One for blood pressure, one for diabetes, one for cholesterol. They don’t always see the full picture. When a patient has five or more meds, adherence drops sharply. The solution? Combination pills, simplified regimens, and better communication between providers. But that takes time-and most visits are only 15 minutes.
Can technology like apps fix medication adherence?
Some apps help-but not for everyone. Older adults, low-income patients, and those with low digital literacy often struggle with apps. A 2023 study found it takes 3-5 training sessions just to learn how to use one. Physical pill organizers with clear labels work better for many. Tech isn’t the answer-it’s one tool. The real fix is simpler: fewer pills, clearer instructions, and better support.
What’s the most effective way to improve adherence?
The best approach combines three things: 1) simplify the regimen (fewer pills, once-daily dosing), 2) automate refills (90-day mail-order), and 3) improve communication (pharmacist counseling). When these are used together, adherence improves by 20-25%. No single fix works alone. It’s about removing barriers, not adding pressure.
What Comes Next?
The healthcare system is slowly waking up. In January 2024, Medicare started paying providers bonuses for hitting adherence targets. Pharmacies are syncing refills. Drugmakers are releasing once-weekly versions of pills. But real change won’t come from tech alone.
It will come when we stop asking patients to be perfect-and start designing systems that work for humans.