Understanding the Connection Between Osteoporosis and Rheumatoid Arthritis
As someone who is constantly researching and writing about health issues, I've come across many topics that are related to one another. Today, I want to explore the relationship between two common conditions: osteoporosis and rheumatoid arthritis. These conditions affect millions of people worldwide, and understanding how they are connected can help us better manage and treat them.
What is Osteoporosis?
Osteoporosis is a bone disease characterized by a decrease in bone density, which leads to weakened bones that are more prone to fractures. This condition can affect anyone, but it is more common in older adults, especially women who have gone through menopause. As we age, our body's ability to create new bone slows down, leading to a higher risk of developing osteoporosis.
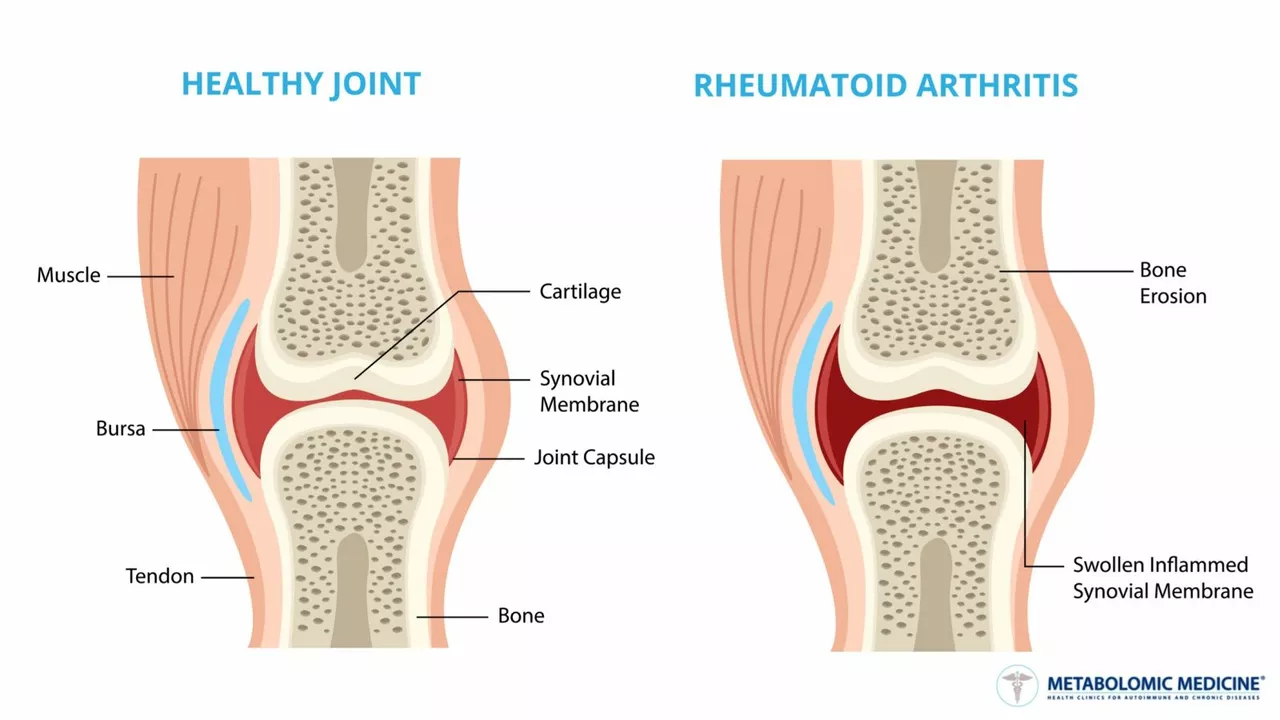
What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is an autoimmune disease that causes inflammation in the joints, leading to pain, stiffness, and swelling. This chronic condition affects more than just the joints, as it can also impact other organs and systems in the body. The exact cause of RA is unknown, but it is believed to involve a combination of genetic and environmental factors.
How Osteoporosis and Rheumatoid Arthritis are Linked
Both osteoporosis and rheumatoid arthritis are conditions that affect the bones and joints, but their connection goes beyond that. Research has shown that people with rheumatoid arthritis are more likely to develop osteoporosis. This is because the inflammation caused by RA can interfere with the normal process of bone remodeling, leading to a decrease in bone density.
The Role of Inflammation in Bone Health
Inflammation is a natural response of our immune system to protect our body from harmful substances, such as bacteria and viruses. However, in rheumatoid arthritis, the immune system mistakenly attacks the body's own tissues, causing inflammation in the joints. This chronic inflammation can affect bone health by disrupting the balance between bone formation and bone resorption, leading to a decrease in bone density and an increased risk of osteoporosis.
Medications and Their Impact on Bone Health
Some medications used to treat rheumatoid arthritis can also contribute to bone loss, further increasing the risk of osteoporosis. For example, corticosteroids, which are commonly prescribed to reduce inflammation, can have a negative impact on bone health. Long-term use of these medications can lead to a decrease in bone density and an increased risk of fractures. It is essential to discuss the potential risks and benefits of medications with your doctor and to closely monitor your bone health while taking these drugs.
Preventing and Managing Osteoporosis in Rheumatoid Arthritis Patients
Since individuals with rheumatoid arthritis have an increased risk of developing osteoporosis, it is crucial to take steps to prevent and manage bone loss. Some ways to promote bone health include:
- Maintaining a diet rich in calcium and vitamin D
- Engaging in regular weight-bearing exercises
- Quitting smoking and limiting alcohol consumption
- Discussing bone-protecting medications with your doctor
Monitoring Bone Density in Rheumatoid Arthritis Patients
Regular bone density tests can help individuals with rheumatoid arthritis monitor their bone health and detect early signs of osteoporosis. These tests, known as dual-energy X-ray absorptiometry (DXA) scans, measure the amount of mineral content in your bones and can help your doctor determine your risk of fractures and develop a personalized treatment plan.
Understanding the Importance of Early Detection and Treatment
Early detection and treatment of both rheumatoid arthritis and osteoporosis can help reduce the risk of complications, such as fractures and joint damage. If you are experiencing symptoms of either condition, it is essential to speak with your doctor as soon as possible. By working together, you can develop a comprehensive treatment plan that addresses both your joint health and your bone health.
Conclusion
In conclusion, understanding the relationship between osteoporosis and rheumatoid arthritis is essential for those affected by either condition. By taking steps to prevent and manage bone loss, monitoring bone density, and seeking early detection and treatment, individuals with rheumatoid arthritis can reduce their risk of developing osteoporosis and improve their overall health and well-being.
Johnny X-Ray
June 18, 2023 AT 16:11Wow, what a powerful overview! Your enthusiasm really shines through, and it’s uplifting to see how you connect the dots between RA and osteoporosis 😊. Keep spreading this hopeful vibe, it truly makes a difference for readers.
tabatha rohn
June 20, 2023 AT 23:44Honestly, the article flirts with oversimplification-mixing complex immunology with basic diet tips feels lazy 😠. A more rigorous approach would’ve earned credibility.
Mark Rohde
June 23, 2023 AT 07:18It's a rollercoaster ride of facts 🎢💥
Rajan Desai
June 25, 2023 AT 14:51The inflammatory cytokine cascade, particularly IL-6 and TNF‑α, directly stimulates osteoclastogenesis, thereby reducing bone mineral density. This mechanistic link is well documented in peer‑reviewed rheumatology studies.
S O'Donnell
June 27, 2023 AT 22:24In reviewing the extant literature, one observes a consistent pattern whereby rheumatoid arthritis predisposes patients to accelerated bone loss. The underlying pathophysiology involves chronic systemic inflammation, which perturbs the delicate equilibrium between osteoblastic bone formation and osteoclastic bone resorption. Moreover, glucocorticoid therapy, a mainstay in RA management, exerts deleterious effects on calcium metabolism and collagen synthesis. Patients receiving prolonged corticosteroid regimens exhibit a marked decline in serum calcium levels, prompting secondary hyperparathyroidism. This endocrine response further amplifies osteoclastic activity, culminating in vertebral and hip fractures. Epidemiological data from multinational cohorts indicate that the incidence of osteoporosis in RA cohorts exceeds that of age‑matched controls by up to thirty percent. Radiographic assessments, particularly dual‑energy X‑ray absorptiometry, reveal reduced t‑scores commensurate with disease severity. Importantly, early implementation of disease‑modifying antirheumatic drugs appears to mitigate inflammatory cytokine load and thus decelerate bone demineralization. Nutritional interventions, including adequate intake of calcium (1200 mg/day) and vitamin D (800‑1000 IU/day), constitute a cornerstone of preventative strategy. Weight‑bearing exercises, such as brisk walking or resistance training, have demonstrable benefits in enhancing bone mineral density. Smoking cessation and moderation of alcohol consumption further reduce ancillary risk factors. Clinicians should adopt a multidisciplinary approach, integrating rheumatology, endocrinology, and physiotherapy expertise. Patient education remains pivotal; individuals must be apprised of the latent risks and empowered to adhere to therapeutic regimens. In summation, the confluence of inflammatory mediators, pharmacologic agents, and lifestyle factors coalesce to heighten osteoporosis susceptibility in rheumatoid arthritis. A proactive, evidence‑based management plan is indispensable to attenuate morbidity and improve quality of life.
Yamunanagar Hulchul
June 30, 2023 AT 05:58What a dazzling fusion of science and self‑care, dear author, your list of preventive measures sparkles with brilliance, offering calcium‑rich delights, vitamin‑D sunshine, weight‑bearing wonders, and smoking‑free serenity, all wrapped in a supportive hug for the reader, truly inspiring, keep it up! 🌟
Sangeeta Birdi
July 2, 2023 AT 13:31It’s heart‑warming to see such compassion; many patients feel isolated, and your guidance offers a gentle beacon of hope 😊. Knowing you’ve considered both medical and emotional aspects truly validates their journey.
Chelsea Caterer
July 4, 2023 AT 21:04Health is a balance of mind, body, and community; addressing RA without bone health is like reading half a story.
Lauren Carlton
July 7, 2023 AT 04:38While the article is informative, the phrase “A higher risk of developing osteoporosis” should be “a higher risk of developing osteoporosis.” Also, “disrupting the balance” would read better as “disrupts the balance.” Minor edits, but they polish the piece.
Katelyn Johnson
July 9, 2023 AT 12:11Great points all around, I love how the community vibe shines through, and the inclusive tone makes everyone feel welcome.
Elaine Curry
July 11, 2023 AT 19:44Honestly i think your personal story about your grandma’s fracture would’ve added a real touch, plus maybe share your own meds list so we can learn more
Patrick Fortunato
July 14, 2023 AT 03:18Look mate, the science is universal, but we’ve got to remember our own health systems do better when they fund early screening, no doubt.
Manisha Deb Roy
July 16, 2023 AT 10:51Pro tip: schedule your DXA scan during the same month each year to track subtle changes; plus, ask your rheumatologist about bisphosphonates if you’re on steroids. Small steps make big differences!
Helen Crowe
July 18, 2023 AT 18:24Keep crushing it!