Stress and Ulcer Risk Calculator
Your risk assessment will appear here after calculation.
Ever wondered whether a hectic workday could literally burn a hole in your gut? The idea that stomach ulcer pain might be stress‑related has lingered for decades, but modern medicine finally pinpoints how the mind and belly interact. This article untangles the biology, reviews the latest research, and gives you practical steps to keep stress from turning into an ulcer.
Quick Facts
- Stress alone rarely causes an ulcer, but it can worsen existing ones.
- Helicobacter pylori infection and NSAID use remain the top two causes.
- Cortisol spikes increase gastric acid secretion and reduce stomach lining protection.
- Managing stress can lower ulcer recurrence by up to 30% in some studies.
- Seek medical help if you have persistent pain, vomiting blood, or unexplained weight loss.
What Is a Stomach Ulcer?
Stomach ulcer is a type of peptic ulcer that forms on the lining of the stomach, causing a sore that can bleed or perforate. It affects roughly 10% of adults worldwide, with higher rates in smokers and older adults. The ulcer develops when the protective mucus layer breaks down, exposing raw tissue to harsh gastric acid.
Classic Causes of Peptic Ulcer Disease
Before diving into stress, it helps to know the two heavy hitters that doctors first look for:
- Helicobacter pylori is a spiral‑shaped bacterium that colonises the stomach, weakening mucus and triggering inflammation.
- Non‑steroidal anti‑inflammatory drugs (NSAIDs) such as ibuprofen or aspirin inhibit prostaglandins, which normally help maintain the mucus barrier.
Both factors can act alone or together, accounting for about 70‑80% of ulcer cases in clinical cohorts.
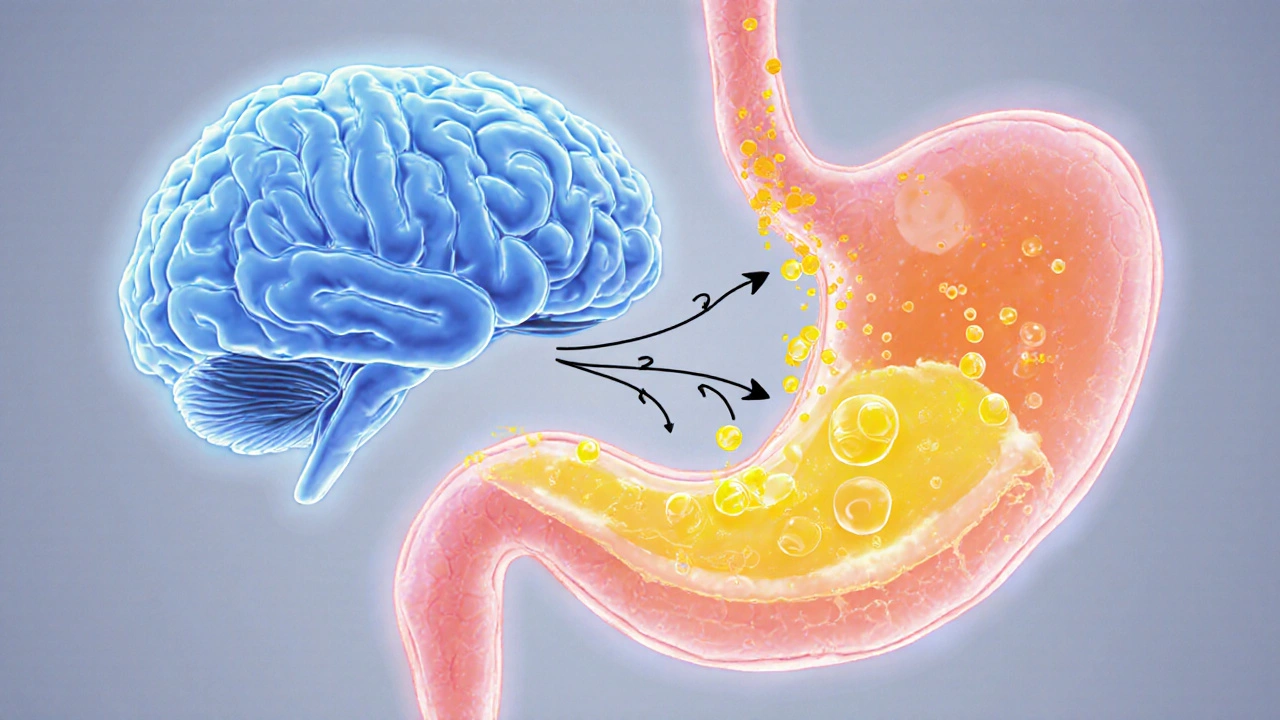
How Stress Affects Your Stomach
When you’re stressed, the brain fires the hypothalamic‑pituitary‑adrenal (HPA) axis, releasing cortisol a steroid hormone that prepares the body for ‘fight or flight’. Cortisol does three things that matter for ulcer formation:
- Stimulates parietal cells to pump more gastric acid hydrochloric acid that aids digestion, raising the acidic load on the stomach lining.
- Suppresses prostaglandin synthesis, weakening the mucus barrier that normally shields the epithelium.
- Alters gut motility via the vagus nerve the main parasympathetic conduit between brain and gut, leading to delayed emptying and increased acid exposure.
Beyond hormones, chronic stress can drive poor lifestyle choices-excess alcohol, smoking, irregular meals-each of which independently raises ulcer risk.
Research Findings: Stress‑Ulcer Link
Historical data from World War II showed “stress ulcers” in soldiers under extreme combat pressure. Modern studies refine that picture:
- A 2022 meta‑analysis of 18 prospective cohorts (over 200,000 participants) found a 1.6‑fold higher odds of ulcer recurrence among individuals reporting high perceived stress.
- Animal models demonstrate that chronic restraint stress doubles gastric ulcer incidence, even when H.pylori is absent.
- Clinical trials using mindfulness‑based stress reduction (MBSR) reported a 25% reduction in ulcer‑related pain scores after 8 weeks.
These findings suggest stress is not a primary cause, but a potent accelerator-especially when the stomach’s defenses are already compromised.
Distinguishing Stress‑Related Ulcers from Other Types
Physicians use a combination of history, endoscopy, and tests to tease apart causes:
- Positive H. pylori breath test or stool antigen points to bacterial involvement.
- Regular NSAID use recorded in medication history flags drug‑induced ulcers.
- High scores on validated stress questionnaires (e.g., Perceived Stress Scale) coupled with no other risk factors may suggest a stress‑linked ulcer.
Endoscopic appearance often looks similar, so treatment decisions rely heavily on identifying and removing the underlying trigger.
Managing Stress to Reduce Ulcer Risk
Even if stress isn’t the sole culprit, cutting its impact can protect your stomach. Here are evidence‑backed tactics:
- Mind‑body practices: Daily 10‑minute breathing exercises lower cortisol by up to 30% (Harvard Health, 2023).
- Regular physical activity: Moderate aerobic workouts improve gut motility and reduce stress hormones.
- Sleep hygiene: Aim for 7‑8hours; sleep deprivation spikes cortisol and gastric acid.
- Diet tweaks: Limit caffeine and spicy foods that can irritate an already inflamed lining.
- Avoid NSAIDs when possible: Opt for acetaminophen or topical analgesics for pain.
- Quit smoking: Nicotine reduces mucus production and increases acid secretion.
When lifestyle changes aren’t enough, doctors may prescribe proton pump inhibitors (PPIs) to suppress acid while you address stressors.
When to Seek Medical Help
Not all tummy aches deserve a doctor’s visit, but watch for these red flags:
- Sharp, burning pain that persists for more than a few days.
- Vomiting blood or material that looks like coffee grounds.
- Black, tarry stools indicating hidden bleeding.
- Unexplained weight loss or loss of appetite.
- Sudden increase in pain after taking NSAIDs.
Early endoscopic evaluation can confirm an ulcer, test for H.pylori, and guide treatment.
| Trigger | Primary Mechanism | Typical Contribution (%) |
|---|---|---|
| Helicobacter pylori | Disrupts mucus, induces inflammation | 45‑60 |
| NSAIDs | Inhibits prostaglandins, erodes protection | 15‑30 |
| Stress (high cortisol) | Increases acid, lowers mucus, slows healing | 5‑15 |
| Smoking | Reduces bicarbonate, impairs blood flow | 10‑20 |
| Alcohol | Irritates lining, raises acid output | 5‑10 |
Frequently Asked Questions
Can stress alone create a stomach ulcer?
Stress by itself rarely initiates an ulcer, but chronic high‑stress states can weaken the stomach’s defenses and accelerate ulcer formation, especially if other risk factors exist.
How does cortisol affect gastric acid?
Cortisol stimulates parietal cells to secrete more hydrochloric acid, raising the stomach’s acidity and increasing the chance that the mucosal lining gets damaged.
Is it safe to take antacids if I’m stressed?
Antacids provide temporary relief, but they don’t address the underlying cause. For chronic stress, combine acid‑suppressing medication with stress‑management strategies.
Can quitting smoking offset stress‑related ulcer risk?
Yes. Smoking cuts mucus production and reduces blood flow to the stomach. Quitting can lower ulcer risk by up to 30%, which also helps mitigate the impact of stress.
What diagnostic test confirms an ulcer caused by stress?
There’s no specific test for “stress‑induced” ulcers. Doctors rely on endoscopy to visualize the ulcer, rule out H.pylori and NSAID use, and assess the patient’s stress level through questionnaires.
How long does it take for an ulcer to heal after stress reduction?
With proper medication and a sustained stress‑management plan, most ulcers begin to heal within 4‑6 weeks. Full healing can take up to 12 weeks.

Bruce T
October 1, 2025 AT 15:36Stress is the silent killer of your gut, and you should quit making excuses.
Mike Rosenstein
October 9, 2025 AT 14:06While stress certainly plays a role, the literature emphasizes a multifactorial etiology. Chronic stress can elevate gastric acid secretion and impair mucosal defenses, thereby increasing ulcer susceptibility. It is also essential to consider NSAID intake, H. pylori infection, and lifestyle habits such as smoking and alcohol consumption. Reducing perceived stress through mindfulness or regular exercise can be a valuable adjunct to medical therapy. Ultimately, a holistic approach yields the best outcomes.
Ada Xie
October 17, 2025 AT 12:36The association between psychosocial stressors and peptic ulcer disease has been substantiated by multiple peer‑reviewed studies. Nonetheless, it is imperative to distinguish correlation from causation when interpreting epidemiological data. Accordingly, clinicians should assess stress levels alongside established risk factors.
Stephanie Cheney
October 25, 2025 AT 11:06Managing stress doesn't have to be a solo mission; simple breathing exercises or short walks can lower cortisol and give your stomach a break. Pairing those habits with a balanced diet and adequate sleep often makes a noticeable difference in ulcer risk.
Georgia Kille
November 2, 2025 AT 08:36👍 Try a 5‑minute diaphragmatic breathing session before meals!
Jeremy Schopper
November 10, 2025 AT 07:06Stress triggers the hypothalamic‑pituitary‑adrenal axis; consequently, cortisol spikes; these spikes can compromise the gastric mucosal barrier; hence, ulcer formation becomes more likely; integrating stress‑reduction techniques-such as yoga or progressive muscle relaxation-into daily routines is advisable.
liza kemala dewi
November 18, 2025 AT 05:36The pathophysiological cascade initiated by chronic psychosocial stress begins with the activation of the sympathetic nervous system, a response that is both rapid and pervasive.
Subsequent release of catecholamines not only raises systemic blood pressure but also stimulates gastric parietal cells to increase hydrochloric acid output.
Elevated acid levels, when unopposed by sufficient bicarbonate secretion, erode the protective mucus layer that normally shields the epithelium.
Concomitantly, stress induces a reduction in mucosal blood flow, thereby impairing the delivery of essential nutrients and reparative cells to the gastric lining.
This hypoxic environment further compromises the integrity of the mucosal barrier, making it more susceptible to invasion by pathogenic organisms such as Helicobacter pylori.
Moreover, the stress‑induced surge in cortisol exerts immunomodulatory effects that can blunt the host’s ability to mount an effective inflammatory response against H. pylori, allowing the bacterium to persist.
When non‑steroidal anti‑inflammatory drugs are added to this milieu, cyclooxygenase inhibition reduces prostaglandin synthesis, which otherwise promotes mucus and bicarbonate secretion.
The cumulative impact of these mechanisms-hyperacidic secretions, diminished mucosal defenses, and impaired immunity-creates an optimal setting for ulcerogenesis.
Epidemiological data support this synergy, demonstrating a statistically significant increase in ulcer incidence among individuals reporting high perceived stress scores combined with regular NSAID use.
Clinicians therefore recommend a multifaceted management plan that addresses both physiological and psychological contributors.
Behavioral interventions such as cognitive‑behavioral therapy, mindfulness meditation, and regular aerobic exercise have been shown to lower perceived stress levels by up to 30 percent in controlled trials.
Pharmacologic therapy should include proton‑pump inhibitors to suppress acid production while eradication regimens target H. pylori whenever present.
Patients are also advised to eliminate modifiable lifestyle risk factors, including smoking cessation and limiting alcohol intake, which independently exacerbate mucosal damage.
Nutritional counseling that emphasizes a diet rich in antioxidants and low in irritants such as spicy foods can further aid mucosal healing.
In summary, while stress alone is rarely the sole cause of a gastric ulcer, its role as a potent accelerator of underlying pathology warrants serious attention in both prevention and treatment strategies.
Jay Jonas
November 26, 2025 AT 04:06Man, I always thought stress was just in my head, but then my stomach started throwing up fireworks after that deadline. Even my doctor said the ulcers were stress‑related, and now I’m seriously reconsidering my coffee habit.
Liam Warren
December 4, 2025 AT 02:36From a gastroenterological perspective, sustained cortisol elevation can precipitate dysregulation of the mucosal protective factor cascade, thereby increasing the propensity for erosive lesions.
Brian Koehler
December 12, 2025 AT 01:06Stress, in concert with ulcerogenic agents, orchestrates a symphony of pathological events; each note-be it acid hypersecretion or mucosal hypoperfusion-contributes to the final crescendo of ulcer formation.
Dominique Lemieux
December 19, 2025 AT 23:36It’s amusing how many people blame “stress” without looking at their daily NSAID consumption. The data clearly show that the combination is far more dangerous than stress alone. Moreover, smoking and alcohol are often ignored in these simplistic narratives. If you’re serious about prevention, you need to address all risk factors, not just the buzzword. The literature is stacked against the “stress‑only” argument, and yet it persists. In short, a balanced lifestyle beats vague optimism every time.
Laura MacEachern
December 27, 2025 AT 22:06Remember, taking small steps to manage stress can have big rewards for your gut health. Even a five‑minute mindfulness break each day can cut cortisol spikes.
BJ Anderson
January 4, 2026 AT 20:36If you ignore the stress factor, you're practically inviting ulcer development; it's not a myth, it's biochemistry. A few lifestyle tweaks can change the whole picture.
Alexander Rodriguez
January 12, 2026 AT 19:06Research shows that individuals with a perceived stress score above 7 have a 20% higher likelihood of developing a peptic ulcer, all else being equal.
Welcher Saltsman
January 20, 2026 AT 17:36Just cut the coffee and try walking more it works.
april wang
January 28, 2026 AT 16:06When I first read about the stress‑ulcer connection, I was skeptical, but a deeper dive into the physiological mechanisms changed my perspective. Chronic activation of the hypothalamic‑pituitary‑adrenal axis leads to sustained cortisol release, which in turn compromises the gastric mucosal barrier. Simultaneously, stress can alter gut motility, promoting stasis and increasing exposure of the epithelium to corrosive acid. Adding to this, behavioral factors such as increased smoking or alcohol consumption during high‑stress periods exacerbate the problem. The evidence suggests that an integrative approach-addressing both psychological stressors and traditional ulcer risk factors-yields the most effective outcomes. Simple interventions like regular aerobic exercise, adequate sleep, and mindfulness practices have been shown to reduce perceived stress scores significantly. While these changes require commitment, the payoff in reduced ulcer risk and overall well‑being is substantial.
Vishnu Raghunath
February 5, 2026 AT 14:36Oh great, another stress‑ulcer link, just what the world needed.