Tendon Rupture Risk Calculator
Your Risk Assessment
Risk Levels
*This calculator is for educational purposes only. Always consult your doctor for medical advice.
Results
What You Should Know
Important: Tendon rupture from fluoroquinolones and steroids can occur within days of starting treatment. Even short courses (5-7 days) can be dangerous when combined with corticosteroids.
Age Factor: Risk doubles for patients over 60. Most ruptures occur in older adults.
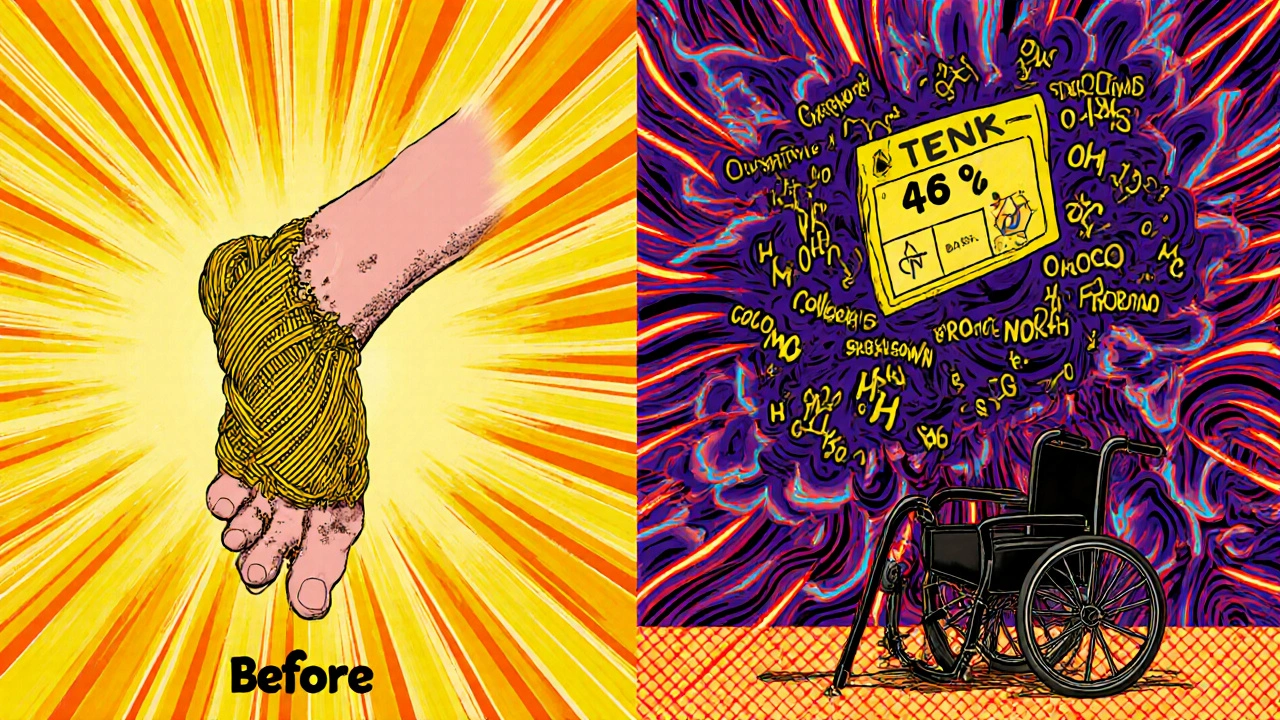
Key Insight: The combination increases rupture risk by 46 times compared to taking either drug alone.
Warning Signs: Pain, swelling, warmth around Achilles tendon, shoulder, or wrist. If you experience sudden sharp pain, stop activity immediately and contact your doctor.
Why a Simple Antibiotic Prescription Could Lead to a Torn Tendon
You take a course of ciprofloxacin for a stubborn urinary tract infection. A week later, you’re walking to the mailbox and hear a loud pop. Your heel goes numb. You can’t push off your foot. You’ve just had an Achilles tendon rupture-and it wasn’t an accident. It was a side effect you were never warned about.
This isn’t rare. Between 2007 and 2012, New Zealand’s adverse drug reporting system recorded 53 cases of tendon damage linked to fluoroquinolone antibiotics. Of those, 36 were full ruptures. Most happened in people over 60. And nearly all of them were taking steroids at the same time.
Fluoroquinolones-drugs like ciprofloxacin, levofloxacin, and norfloxacin-are powerful antibiotics. They work by breaking down bacterial DNA. But they don’t just target bacteria. They also mess with human collagen, the protein that holds tendons together. And when you add corticosteroids into the mix, the damage multiplies.
The Perfect Storm: Fluoroquinolones + Steroids
Let’s be clear: fluoroquinolones alone raise your risk of tendon rupture. Studies show a 1.7-fold increase in tendinitis and a 1.3-fold increase in full rupture. But when you combine them with oral or injected steroids-like prednisone or methylprednisolone-the risk jumps to 46 times higher than if you took either drug alone.
This isn’t theoretical. In a 2000 JAMA Internal Medicine study, researchers found that patients over 60 who took both a fluoroquinolone and a corticosteroid were 46 times more likely to rupture their Achilles tendon than those taking neither. The same study estimated that 2% to 6% of all Achilles ruptures in older adults were directly caused by this drug combo.
Why does this happen? Corticosteroids weaken tendons by suppressing collagen production. Fluoroquinolones make it worse. They trigger oxidative stress in tendon cells, disrupt mitochondrial function, and increase enzymes that break down connective tissue. Together, they turn a healthy tendon into a frayed rope-ready to snap under normal stress.
Who’s Most at Risk?
Not everyone who takes these drugs will have a problem. But certain people are sitting on a ticking clock.
- Age 60+: Risk of rupture doubles compared to younger adults. Tendons naturally lose elasticity with age, and healing slows down.
- On oral or injectable steroids: Even short courses (5-7 days) can be dangerous when paired with fluoroquinolones.
- History of tendon injury: If you’ve had a prior rupture or tendinitis, your tendons are already vulnerable.
- Chronic kidney disease: Especially with eGFR below 30 mL/min. Fluoroquinolones are cleared by the kidneys. Poor clearance means higher drug levels and more damage.
- Diabetes: High blood sugar weakens collagen structure. Add a fluoroquinolone? You’re stacking the deck.
- Organ transplant recipients: These patients are almost always on long-term steroids. Fluoroquinolones are often used to prevent infection-but the combo is deadly for tendons.
One case report described a 72-year-old man with diabetes and kidney disease. He took ciprofloxacin for a bladder infection and prednisone for a flare-up of rheumatoid arthritis. Five days later, he ruptured both Achilles tendons-simultaneously. He needed surgery on both feet. He’s still using a cane two years later.

Which Antibiotics Are the Worst?
All fluoroquinolones carry this risk. But some are more dangerous than others.
Ciprofloxacin is the most commonly reported culprit. In New Zealand’s reporting system, it accounted for 68% of all tendon injury cases between 2007 and 2012. Norfloxacin came second at 30%. Levofloxacin and moxifloxacin are also linked, but less frequently.
Why ciprofloxacin? It’s widely prescribed, often overused. It’s also highly concentrated in tendon tissue. Studies show it binds more strongly to collagen than other fluoroquinolones, disrupting its structure faster.
Compare this to other antibiotics: penicillins, cephalosporins, azithromycin. None have been linked to tendon rupture in any meaningful study. If you’re at risk, ask your doctor: Is there a safer antibiotic?
When Does It Happen?
You might think side effects show up after weeks of use. Not with fluoroquinolones.
The median time to first symptoms-pain, swelling, stiffness-is just 6 days. Eighty-five percent of cases occur within the first month. And here’s the kicker: half of all ruptures happen after you’ve stopped taking the drug.
That means you could finish your pills on Friday, feel fine over the weekend, and tear your tendon on Monday morning while walking your dog. There’s no warning. No gradual buildup. Just sudden, sharp pain and loss of function.
Some patients report a "pop" or "snap." Others feel like they’ve been kicked in the heel. Many can’t stand on their toes afterward. It’s not a strain. It’s a complete tear.
What to Do If You’re Already Taking Both
If you’re on a fluoroquinolone and a corticosteroid right now, don’t panic-but don’t ignore it either.
- Stop exercising. No running, jumping, stair climbing, or heavy lifting. Even walking too much can stress a weakened tendon.
- Watch for early signs. Pain, warmth, or swelling around your Achilles, shoulder, or hand tendons. Even mild discomfort is a red flag.
- Call your doctor immediately if you feel sudden pain. Don’t wait for it to get worse.
- Don’t stop antibiotics on your own. But do ask: Can I switch to a safer drug? Sometimes, a 5-day course of amoxicillin-clavulanate can replace ciprofloxacin for a UTI.
Many doctors still prescribe this combo without thinking twice. If your doctor says, "It’s rare," ask: "What’s the exact risk if I’m 70 and on prednisone?" If they can’t answer, get a second opinion.
What’s the Long-Term Impact?
A torn Achilles tendon isn’t like a sprained ankle. Recovery takes 6 to 12 months. Many people never fully regain their strength.
Surgery is often required. Even then, you’ll need months of physical therapy. Up to 50% of patients develop problems in both tendons. Some end up with chronic pain, reduced mobility, or even permanent disability.
One study followed 34 patients who ruptured their Achilles after taking fluoroquinolones. Five years later, 40% still had pain during daily activities. Only 30% returned to their pre-injury activity level.
And this isn’t just about physical recovery. It’s about independence. Older adults who rupture a tendon often lose the ability to live alone. They need home care. They fall more. Their quality of life plummets.
How Doctors Are Changing Their Approach
In 2013, the U.S. FDA added a "black box" warning-the strongest possible-to all systemic fluoroquinolones. It says: Do not use for uncomplicated infections like sinusitis, bronchitis, or simple UTIs if other options exist.
That changed prescribing. Fluoroquinolone use dropped by nearly 30% in the U.S. after the warning. In Australia, guidelines now say: Never use fluoroquinolones in patients over 60 on steroids unless there’s no alternative.
Doctors are learning. But not fast enough. A 2022 study in the Journal of Antimicrobial Chemotherapy found that 1 in 5 older patients still got fluoroquinolones for simple UTIs-even though nitrofurantoin or fosfomycin are safer and just as effective.
Bottom line: fluoroquinolones are not first-line anymore. They’re last-resort drugs. If your infection isn’t life-threatening, don’t risk your tendons.
What You Can Do Now
- Ask before you take it: "Is this fluoroquinolone necessary? Are there safer options?"
- Check your meds: If you’re on prednisone, methylprednisolone, or dexamethasone, don’t accept a fluoroquinolone without a clear plan.
- Know the signs: Pain, swelling, or stiffness in your heel, shoulder, or wrist? Stop activity. Call your doctor.
- Report it: If you or someone you know has a tendon rupture after taking these drugs, report it to your national drug safety agency. It helps others.
This isn’t about fear. It’s about awareness. Fluoroquinolones save lives in serious infections like pneumonia, sepsis, or complicated kidney infections. But they’re not harmless. And when paired with steroids, the risk isn’t just real-it’s devastating.
Don’t assume your doctor knows. Don’t assume it won’t happen to you. Tendon rupture from this combo is rare-but when it happens, it changes your life forever.
Can you get tendon rupture from one dose of a fluoroquinolone?
Yes. While most cases occur after several days of use, there are documented cases of tendon rupture after just one or two doses. Symptoms can appear within hours or days. This is why even short courses require caution, especially in high-risk patients.
Are topical steroids safe with fluoroquinolones?
Topical steroids (creams, lotions) are generally considered low risk because very little enters the bloodstream. However, if you’re using them over large areas of skin, for long periods, or on broken skin, systemic absorption can occur. When in doubt, avoid combining them with fluoroquinolones unless your doctor confirms it’s safe.
Is there a blood test to check for tendon damage from these drugs?
No. There’s no reliable blood test to predict or detect early tendon damage from fluoroquinolones. The damage happens at the tissue level, not through measurable biomarkers. That’s why symptoms like pain and swelling are your only warning signs-and why early recognition is critical.
What are safer alternatives to fluoroquinolones for UTIs?
For uncomplicated urinary tract infections, nitrofurantoin, fosfomycin, and trimethoprim-sulfamethoxazole are preferred. They’re just as effective, don’t carry tendon risks, and are recommended by guidelines in the U.S., Europe, and Australia. Fluoroquinolones should only be used if these fail or aren’t suitable.
Can tendon damage from fluoroquinolones be reversed?
Once a tendon ruptures, it can’t be fully restored to its original strength. Surgery and rehab can help you regain function, but many people experience lasting weakness, stiffness, or pain. Prevention is the only true cure. Stopping the drugs early if symptoms appear can prevent rupture-but not reverse existing damage.
Should I avoid fluoroquinolones if I’m over 50?
Not automatically-but you should be extra cautious. Risk increases significantly after 60, but damage has been reported in people as young as 40, especially if they have other risk factors like diabetes, kidney disease, or steroid use. Always ask your doctor if the benefit outweighs the risk.

Herbert Scheffknecht
November 19, 2025 AT 06:22It's wild how we treat medicine like a vending machine-pop a pill, get fixed. But tendons? They don't care about your UTI. They just want to hold you upright. Fluoroquinolones don't just kill bacteria-they unravel the very structure that lets you walk, run, or even stand up from a chair. And steroids? They're the silent partner in crime, quietly turning your collagen into dust. We got scared of opioids, but this? This is the quiet epidemic no one talks about until you're on crutches at 72.
Jessica Engelhardt
November 20, 2025 AT 22:47Martin Rodrigue
November 21, 2025 AT 13:11While the epidemiological data presented is compelling, it is essential to contextualize the absolute risk. The 46-fold relative increase cited in the JAMA study must be interpreted against a baseline incidence of Achilles rupture in the elderly population of approximately 0.02% per year. Even with a multiplicative interaction, the absolute risk remains low. Furthermore, confounding variables such as physical activity levels, comorbidities, and concomitant NSAID use were not fully controlled in most retrospective analyses. The FDA black box warning, while appropriate for risk communication, may have contributed to therapeutic underutilization in cases where fluoroquinolones are clinically indicated.
Sherri Naslund
November 23, 2025 AT 06:20Ashley Miller
November 24, 2025 AT 13:01Lauren Hale
November 26, 2025 AT 11:59I’ve been a nurse for 22 years, and I’ve seen this exact scenario play out too many times. A patient comes in with a UTI, gets cipro because it’s fast and easy, and a week later they’re in the ER with a ruptured tendon. No one warned them. No one even mentioned it. I’ve handed out pamphlets, written notes in charts, asked doctors twice-sometimes they listen, sometimes they roll their eyes. But here’s the thing: if you’re over 60, on steroids, or diabetic, you deserve better than a 10-minute script. Ask for nitrofurantoin. Ask for fosfomycin. Ask like your life depends on it-because it does. And if your doctor says 'it’s rare,' ask them how many cases they’ve seen. If they can’t answer, find someone who can.
Greg Knight
November 27, 2025 AT 10:54Look, I get it. This stuff is terrifying. I had a client-a 68-year-old veteran-who ruptured his Achilles after a 5-day course of cipro for a bladder infection. He was on prednisone for his RA. He’s still rehabbing two years later. But here’s the thing: fear doesn’t help. Action does. If you’re on these meds, don’t just sit there. Track your symptoms. Keep a pain journal. Note any stiffness, warmth, or weird twinges in your heels or shoulders. If you feel something, STOP moving and call your doctor the same day. Don’t wait for the pop. Don’t wait for the swelling. That’s your body screaming. And if your doctor won’t listen? Get a second opinion. There are so many safer options out there. You’re not powerless. You just have to speak up before it’s too late.
rachna jafri
November 27, 2025 AT 15:54