Penicillin Allergy Risk Assessment
This tool helps you understand if your reaction to penicillin might be a true allergy or a common side effect. Remember: only IgE-mediated reactions (like hives, swelling, breathing difficulties within minutes) are true allergies. Most reactions reported as "allergies" are actually side effects that don't require lifelong avoidance.
Important: This is not a medical diagnosis. Always consult a healthcare professional for proper evaluation.
More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the truth: penicillin allergy is often misdiagnosed. In fact, fewer than 1% of those people actually have a real immune system reaction to it. The rest? They’re confusing side effects-common, harmless, and temporary-with something life-threatening. This mistake isn’t just inconvenient. It’s dangerous. And it’s happening to millions.
What’s Really Going On With Penicillin Allergies?
A true penicillin allergy is an immune system response. Your body sees penicillin as an invader and mounts a defense. That’s what triggers symptoms like hives, swelling of the face or throat, trouble breathing, or a sudden drop in blood pressure. These reactions usually happen within minutes to an hour after taking the drug. This is called an IgE-mediated reaction, and it’s the only kind that counts as a real allergy. But here’s where things get messy. Most people who think they’re allergic to penicillin never had a true allergic reaction. They had a rash. Or nausea. Or diarrhea. And someone-maybe a doctor, maybe a parent-called it an allergy. That label stuck. And now, decades later, they’re avoiding penicillin, even though their body might handle it just fine.Side Effects Aren’t Allergies
Side effects are not the same as allergies. They don’t involve your immune system. They’re just how your body reacts to the drug’s chemistry. Think of it like taking aspirin and getting a stomach ache. That’s not an allergy. It’s a side effect. Common penicillin side effects include:- Mild nausea or upset stomach (happens in 5-10% of people)
- Diarrhea (1-2% of users)
- Vaginal yeast infections (due to disruption of normal bacteria)
- Headache or dizziness
- Mild skin rash (often viral in origin, not drug-related)
The Real Danger of a Misdiagnosed Allergy
When you’re labeled allergic to penicillin, doctors can’t use it-even if it’s the best, safest, and cheapest option. Instead, they reach for broader-spectrum antibiotics like vancomycin, clindamycin, or fluoroquinolones. These drugs are stronger, more expensive, and far more likely to cause serious problems. For example:- People with a mislabeled penicillin allergy are 45% more likely to get a Clostridioides difficile infection-a dangerous gut infection that causes severe diarrhea and can be fatal.
- They’re more likely to develop MRSA, a drug-resistant staph infection that’s harder to treat.
- Studies show patients with false allergy labels have 6 more deaths per 1,000 hospitalizations in the year after being labeled.

How Do You Know If It’s Real?
The good news? You can find out. There’s a proven, safe way to test whether you really have a penicillin allergy. The standard process has three steps:- History review. A doctor asks detailed questions: When did the reaction happen? What were the symptoms? Did you need epinephrine? Was it a rash that appeared days later? The PEN-FAST tool helps doctors quickly assess your risk.
- Skin testing. A tiny amount of penicillin is placed under your skin. If you’re truly allergic, you’ll get a red, itchy bump within 15-20 minutes. This test is highly accurate.
- Oral challenge. If skin testing is negative, you take a small dose of amoxicillin (a penicillin-type drug) under supervision. If you tolerate it, you’re cleared. No more allergy label.
Why So Many People Still Believe They’re Allergic
The myth persists for a few reasons. First, many people were labeled allergic as kids. A viral rash during an ear infection? That was called a penicillin allergy. But viruses cause rashes. Penicillin doesn’t. Second, doctors don’t always follow up. If you told your pediatrician you got a rash after penicillin, they wrote it down. But no one ever asked you again. No one ever tested you. Third, fear. People are scared to get tested. They worry they’ll have a reaction. But here’s the thing: in over 50,000 tests done at Mayo Clinic between 2015 and 2022, there were zero serious reactions during the oral challenge.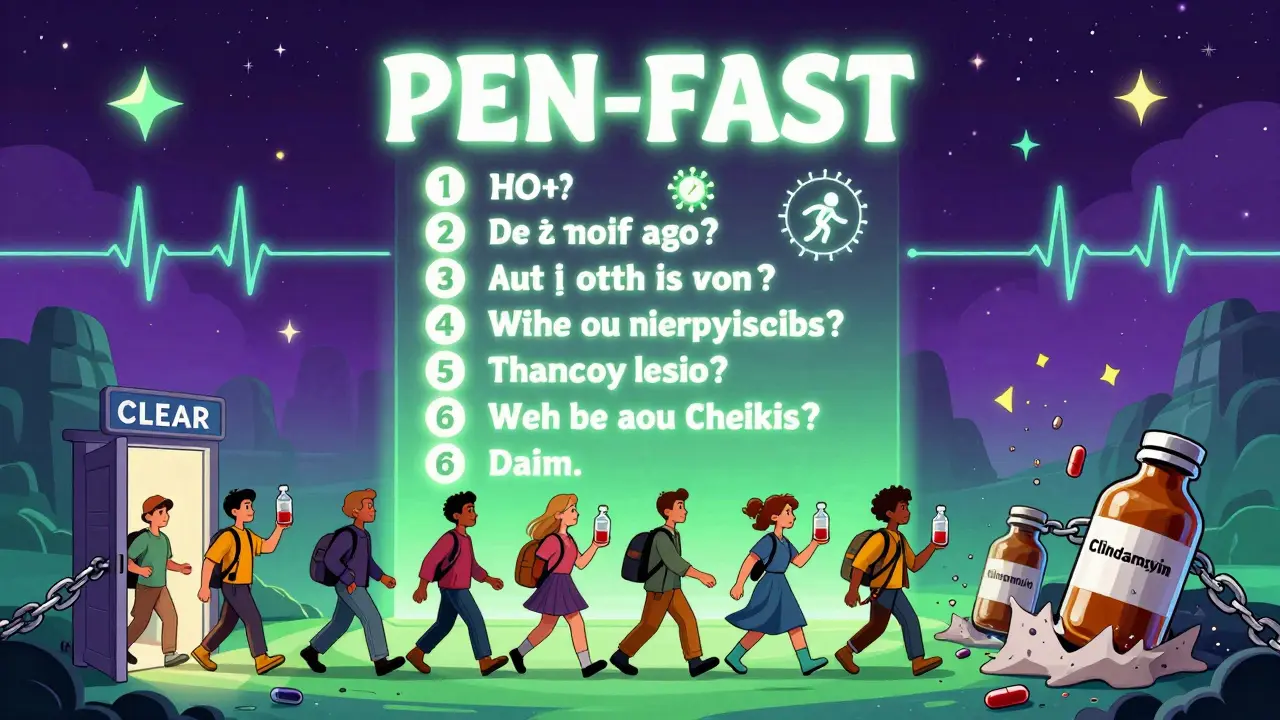
What You Can Do Today
If you’ve been told you’re allergic to penicillin:- Check your records. What exactly happened? Was it a rash? Diarrhea? Anaphylaxis?
- Ask your doctor if you’ve ever been tested. If not, ask for a referral to an allergist.
- Bring up the PEN-FAST tool. It’s a simple questionnaire doctors use to decide if you’re low-risk.
- If you had a reaction more than 10 years ago, you’re even more likely to be cleared. IgE antibodies fade over time. Eighty percent of people lose their allergy after a decade.

Henry Sy
January 15, 2026 AT 03:46So let me get this straight-you’re telling me my mom’s been keeping me away from penicillin since I was five because I got a rash during an ear infection? That’s the same rash I got when I ate strawberries and cried for three hours. And now I’m being prescribed some fancy-pants antibiotic that costs more than my rent? I’m not mad, I’m just disappointed in the medical industrial complex.
Also, can we talk about how every time I say ‘I’m allergic to penicillin,’ doctors look at me like I just admitted I believe in flat earth? Like I’m the weirdo for not wanting to die from a drug I never even tested properly? Yeah, I’m not rushing to swallow it. But hey, if you’re offering a free skin test, I’m in. Just don’t make me sign a waiver that says I won’t sue if I turn into a human balloon.
Anna Hunger
January 15, 2026 AT 17:33It is imperative to recognize that the misclassification of adverse drug reactions as true immunoglobulin E-mediated allergies constitutes a significant clinical and public health concern. The data presented herein are not only statistically robust but also clinically actionable. Patients who are incorrectly labeled as penicillin-allergic are being exposed to increased morbidity and mortality risks due to the substitution of broader-spectrum antimicrobial agents. It is therefore ethically incumbent upon healthcare providers to implement systematic de-labeling protocols, ideally through pharmacist-led allergy clinics, in accordance with evidence-based guidelines established by the American Academy of Allergy, Asthma & Immunology.
Dylan Livingston
January 17, 2026 AT 07:31Oh wow. Another feel-good article from the medical establishment telling us we’re all dumb for surviving childhood. Let me guess-the next thing you’ll say is that vaccines cause autism, but only if you’re too lazy to read the 47-page CDC white paper on it.
So I had a rash after penicillin at age seven? Clearly, that’s just a ‘viral rash.’ And I suppose the fact that I broke out in hives and my tongue swelled up like a balloon? That was just ‘stress.’
Oh wait. You didn’t mention anaphylaxis. Because that’s inconvenient. You want us to believe that 10% of Americans are just delusional? That’s not a medical issue-that’s a propaganda campaign. Who profits when you replace penicillin with $1,200 antibiotics? Hint: not the patient.
And no, I’m not getting tested. I’ve seen what happens to people who question the system. They get labeled ‘non-compliant.’ And then they disappear from the records.
says haze
January 18, 2026 AT 09:35There’s a deeper epistemological crisis here, isn’t there? We’ve outsourced our bodily autonomy to a system that diagnoses us with labels before it even listens. The penicillin allergy myth isn’t just a medical error-it’s a metaphor for how modern medicine has become a linguistic prison. We are not our diagnoses. We are not our rashes. We are not our immune responses. We are the silence between the symptoms.
And yet, we are coerced into believing that a single childhood event, documented by a tired pediatrician in 1997, defines our entire pharmacological future. The real tragedy isn’t the misdiagnosis-it’s the surrender. We’ve allowed institutions to write our bodies for us. And now we’re surprised when those words turn into death sentences.
So yes-get tested. But also ask: who wrote the script? And why did we stop reading between the lines?
Alvin Bregman
January 19, 2026 AT 11:11man i thought i was the only one who got told i was allergic to penicillin cause i got a rash after amoxicillin when i was 6
turns out i had mono and the rash was from the virus not the drug
my doc never followed up and now im stuck with cipro for every infection
just got a new doctor last year and she asked me about it and i was like wait what
im getting tested next month if theyll do it
also why does everyone keep calling it penicillin when they mean amoxicillin theyre not the same thing but everyone just says penicillin like its one magic word
anyone else feel like doctors just write stuff down and forget it
Sarah -Jane Vincent
January 20, 2026 AT 06:40Oh so now the CDC is pushing this because Big Pharma wants us to use more expensive antibiotics? Classic. They’ve been doing this for decades. You think they care about your ‘C. diff’ risk? No. They care about the $20 billion they’re losing because penicillin is cheap. So they’re rewriting history to make you scared of your own immune system.
And who’s funding these ‘de-labeling programs’? Who’s training the pharmacists? Who’s pushing the Epic EHR updates? Hint: it’s not your grandma’s clinic.
I’ve seen the data. The ‘zero serious reactions’ at Mayo? That’s cherry-picked. What about the ones that happened in rural ERs? What about the people who died because they didn’t have access to a ‘proper’ test?
Don’t be fooled. This isn’t science. It’s marketing with a stethoscope.
Jason Yan
January 21, 2026 AT 03:43I love how this article doesn’t just tell you what’s wrong-it gives you a way out. That’s rare. Most health content just scares you and leaves you hanging.
But here’s the real win: you don’t need to be a medical expert to change your story. You just need to ask the right question: ‘Was this really an allergy?’
I had a rash after penicillin in college. I thought I was allergic. Turned out it was poison ivy I touched the same day. My doctor never asked. I never questioned it. I avoided penicillin for 12 years.
Got tested last year. Negative. Took amoxicillin for a sinus infection. Felt fine. Slept better. Didn’t need a $500 antibiotic.
If you’ve been carrying this label for decades, you’re not being careful-you’re being haunted by a ghost. And ghosts don’t pay your medical bills.
Go get checked. Your future self will thank you.
shiv singh
January 21, 2026 AT 13:59you think this is bad wait till you hear about the 5G penicillin conspiracy
they inject nanobots into your blood when you take antibiotics so they can track your emotions
my cousin’s uncle’s neighbor got a penicillin shot and now his dog talks in spanish
and you want me to trust a doctor who works for the government and wears a white coat like it’s a cult uniform
you want me to take a test? what if the test is the trap
the real allergy is to trusting anyone who says ‘trust me’
and also why is everyone from america acting like they invented medicine
we had herbal remedies before your penicillin was even a thought
Robert Way
January 21, 2026 AT 20:17so i had a rash after penicillin and now i cant take it and its pissing me off because my knee infection is getting worse and the only thing theyll give me is cipro and it makes me feel like my insides are melting
but i dont know if i shoud get tested cause what if i die
also i think the doctor who gave me the penicillin was drunk
he wrote my name wrong on the chart
his name was dr. smith but he signed it as dr. smyth
so how can i trust him about my allergy
anyone know if you can get the test done at cvs
Sarah Triphahn
January 23, 2026 AT 01:49Let’s be honest-most people who say they’re allergic to penicillin just hate taking medicine. They don’t want to swallow pills. They don’t want to feel sick. So they invent a story. ‘Oh, I got a rash.’ Really? Or did you just get a sunburn and blame the antibiotic?
And now we’re supposed to believe that 95% of these people are fine? That’s statistically absurd. If it were that easy, why aren’t we doing this for every drug?
Don’t get me wrong-I’m not saying everyone is lying. But the narrative is too clean. Too perfect. Too convenient for the pharmaceutical industry.
And yet, we’re supposed to be grateful for this ‘solution’? No. We’re supposed to be suspicious.
Vicky Zhang
January 23, 2026 AT 02:49I cried when I read this. I’m 32 and I’ve spent my whole life avoiding penicillin because my mom said I had an allergy when I was 4. I had a rash. That’s it. No swelling. No trouble breathing. Just a red spot. But she told me I was allergic and I believed her.
I got strep throat last year and the doctor gave me azithromycin. It made me nauseous for a week. I thought, ‘Why is this so hard?’ Then I read this article. I went to an allergist. Got tested. Negative.
I took amoxicillin two weeks ago. Felt fine. Slept like a baby. Didn’t even need Tylenol.
I feel like I’ve been freed from a prison I didn’t even know I was in. Thank you for writing this. I’m telling everyone I know.
Allison Deming
January 24, 2026 AT 04:41While the intent of this article is commendable, the oversimplification of a complex immunological phenomenon risks fostering a dangerous level of complacency among the general public. The assertion that ‘95% of people are cleared’ is misleading without context: clearance rates are contingent upon rigorous clinical protocols, patient selection, and post-test monitoring. To suggest that all individuals with a self-reported allergy should undergo testing without evaluating the nature of the original reaction is not merely irresponsible-it is potentially life-threatening.
Furthermore, the dismissal of non-IgE-mediated reactions as ‘not real’ ignores the existence of delayed hypersensitivity reactions, which can manifest as severe cutaneous adverse reactions such as Stevens-Johnson syndrome. These are not ‘side effects.’ They are immune-mediated. And they are deadly.
Caution, not convenience, must guide clinical decision-making.
Susie Deer
January 24, 2026 AT 05:23why are we even talking about this
penicillin is for weak people
real americans use garlic and prayer
if you need antibiotics you were already beaten
my grandpa fought in korea and never took a pill
he just drank whiskey and prayed
and he lived to 98
so stop pushing your liberal medicine on us
trust nature not big pharma
and if you die from a rash you deserved it
TooAfraid ToSay
January 24, 2026 AT 15:05in nigeria we don’t have penicillin allergy because we don’t have doctors who can spell it
we just take whatever the chemist gives us
last week i had fever and the man gave me ‘penicillin’ in a plastic bag with no label
i took it
i lived
so maybe the real problem isn’t the allergy
maybe it’s the people who have too many options
and too much time to worry
Henry Sy
January 26, 2026 AT 11:24Wait-so if I get tested and cleared, can I go back to my mom and say ‘sorry, I was wrong, you didn’t raise a hypochondriac, you raised a statistically normal human’?
Because I’ve been avoiding penicillin for 20 years and she still brings it up every time I have a sore throat. ‘Remember when you got that rash?’ Yeah, Mom. I remember. I’ve been carrying it like a scar.
Now I’ve got a doctor’s note saying I’m fine. Do I still have to eat the chicken soup you made for 17 years because ‘it’s natural’?
Also, can I now ask for the $10,000 she owes me for all the expensive antibiotics I’ve paid for? Just a thought.