More than 1 in 3 adults in Australia struggle with sleep at least a few nights a week. For many, the solution feels simple: grab a bottle of OTC sleep aids from the pharmacy shelf. But these little pills aren’t harmless snacks. They’re powerful drugs with real risks - and most people have no idea how dangerous they can be if used the wrong way.
What’s Actually in OTC Sleep Aids?
There are two main types of over-the-counter sleep aids, and they work in completely different ways.
The first group is built around antihistamines - mainly diphenhydramine and doxylamine. These are the same chemicals found in allergy meds like Benadryl and Unisom. They weren’t designed to help you sleep. They cause drowsiness as a side effect. That’s why you feel sleepy after taking them. But your body doesn’t distinguish between “allergy relief” and “sleep aid.” It just reacts to the drug.
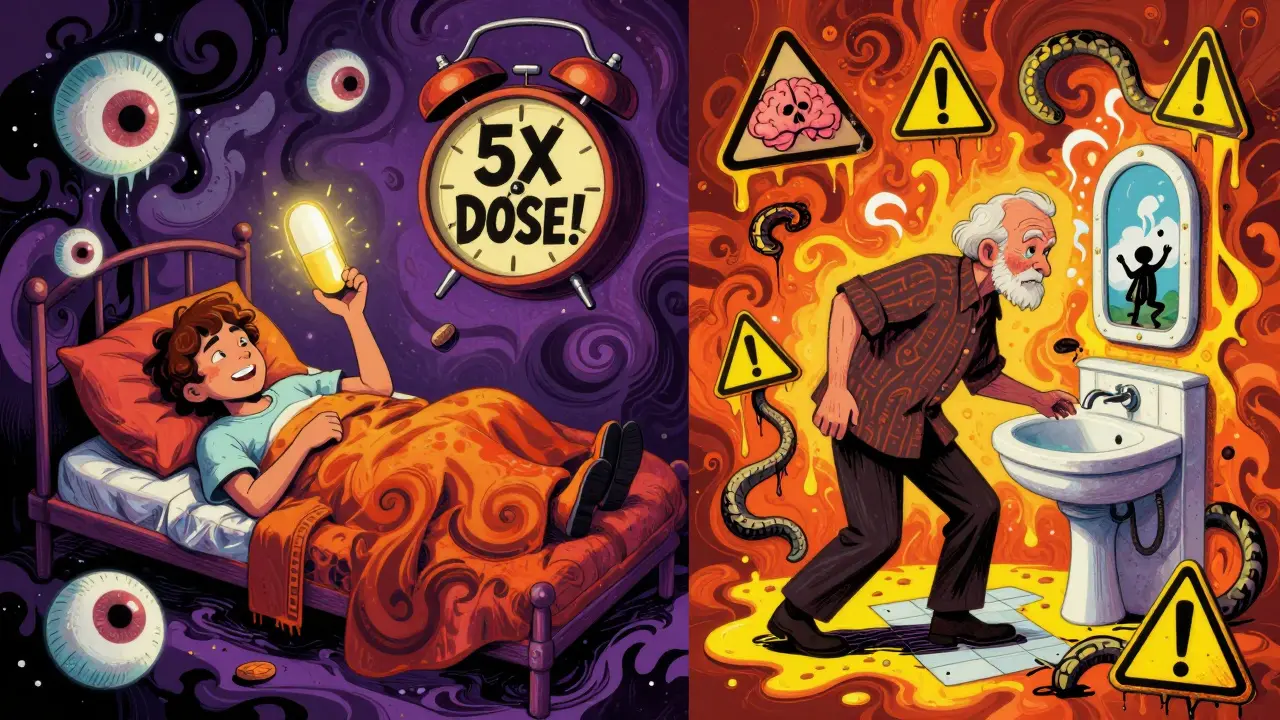
The second group is supplements: melatonin, valerian root, chamomile. These are sold as “natural,” but that doesn’t mean safe. Melatonin is a hormone your brain naturally makes to signal bedtime. Taking it as a pill tricks your body into thinking it’s time to sleep. But here’s the catch: supplements aren’t regulated like real medicine. A 2017 study found that melatonin products contained anywhere from 83% less to 478% more than what was listed on the label. You could be taking a dose five times higher than you think.
How Effective Are They Really?
If you’ve ever read the box, you’ve probably seen claims like “falls asleep faster” or “sleeps through the night.” But the truth? The improvements are tiny.
Studies show these products reduce the time it takes to fall asleep by just 3 to 13 minutes. They add maybe 20 to 60 extra minutes of sleep total. That’s not a full night’s rest. That’s barely enough to feel slightly less exhausted the next day.
And here’s the kicker: they don’t improve sleep quality. You might fall asleep faster, but you’re still missing deep, restorative sleep. That’s the kind your brain needs to repair itself, process memories, and reset your mood. OTC sleep aids don’t fix that.
The Side Effects Nobody Talks About
Antihistamine-based sleep aids - diphenhydramine and doxylamine - are part of a drug class called anticholinergics. These drugs block a brain chemical called acetylcholine. That’s what causes drowsiness. But it also causes a long list of unpleasant and sometimes dangerous side effects:
- Dry mouth (32% of users)
- Blurred vision (18%)
- Constipation (24%)
- Difficulty urinating (especially dangerous for men with prostate issues)
- Confusion and memory problems - especially in people over 65
And here’s the scariest part: long-term use of these drugs is linked to a higher risk of dementia. A 7-year study of over 3,400 people found that those who took anticholinergic medications - including OTC sleep aids - had a 54% higher risk of developing dementia. That’s not a small risk. That’s a major red flag.
Melatonin has its own problems. People think it’s “natural,” so it’s safe. But it’s not. Common side effects include:
- Daytime drowsiness (45% of users)
- Headaches (31%)
- Vivid dreams or nightmares (68%)
- Nausea and dizziness
- Bedwetting in children (8%)
Higher doses (above 5mg) make these worse. And if you take melatonin every night for months, your body can stop making its own. That’s called tolerance. You’ll need more and more just to get the same effect - and then you can’t sleep without it.
Who Should Avoid These Completely?
These aren’t safe for everyone. In fact, they’re dangerous for certain groups:
- People over 65: Antihistamines increase fall risk by 50%. That means broken hips, head injuries, hospital stays. The American Geriatrics Society lists diphenhydramine as a “potentially inappropriate medication” for seniors.
- People with sleep apnea: These drugs relax your throat muscles. That makes breathing interruptions worse during sleep. You could stop breathing more often - or even longer.
- Pregnant or breastfeeding women: There’s not enough data to say melatonin is safe. Diphenhydramine is labeled “Category B,” meaning no proven harm - but also no solid proof it’s safe. Better to avoid it.
- Anyone with glaucoma, enlarged prostate, or liver disease: These conditions can make side effects worse.
How Long Is “Safe” to Use Them?
Every box says: “Do not use for more than two weeks.” But a 2022 survey found that 38% of people use them for longer than that. Nearly 1 in 5 uses them for over a month.
That’s a problem. Why? Because when you stop, your insomnia often comes back worse. That’s called rebound insomnia. About 30% of people who use OTC sleep aids for more than two weeks experience it.
And tolerance builds fast. If you take melatonin every night for 10 days, your body may start needing more to work. You’re not fixing your sleep - you’re creating a dependency.
The real rule? Use them once or twice a week - max. For jet lag, travel, or a really bad night. Not for your regular routine.
What Should You Do Instead?
The best treatment for chronic insomnia isn’t a pill. It’s Cognitive Behavioral Therapy for Insomnia (CBT-I).
CBT-I helps you change the thoughts and habits that keep you awake. It teaches you how to relax your body, manage stress, and reset your internal clock. Studies show it works for 70-80% of people - and the results last. Unlike pills, it doesn’t wear off. You don’t need to keep taking it.
And it’s available online, through apps, or with a therapist. Some Medicare rebates even cover it in Australia.
Other simple fixes work too:
- Get sunlight in the morning - even 10 minutes helps reset your rhythm.
- Stop screens 1 hour before bed. Blue light kills melatonin production.
- Keep your bedroom cool, dark, and quiet.
- Don’t lie in bed awake for more than 20 minutes. Get up, read a book, come back later.
The Bottom Line
OTC sleep aids are not a solution. They’re a Band-Aid on a broken bone.
They might help you fall asleep once or twice. But they don’t fix the root cause. And the longer you use them, the more you risk confusion, falls, memory loss, and dependence.
If you’ve been using them for more than two weeks, it’s time to stop. Not because you’re weak. Because you deserve better sleep - without side effects.
See a doctor. Talk to a sleep specialist. Try CBT-I. Your brain will thank you.
Can I take OTC sleep aids every night?
No. Taking OTC sleep aids every night increases your risk of dependence, tolerance, and serious side effects like confusion, falls, and dementia. Medical guidelines recommend using them for no more than 7-10 days, and never longer than two weeks without seeing a doctor.
Is melatonin safer than diphenhydramine?
Melatonin has fewer immediate side effects than antihistamines, but it’s not safer long-term. It can cause vivid dreams, daytime drowsiness, and tolerance. Plus, since it’s not regulated, you might be taking 5x the dose you think. Antihistamines carry a higher risk of dementia and falls, especially in older adults. Neither is meant for daily, long-term use.
Why do I feel groggy all day after taking OTC sleep aids?
Antihistamines like diphenhydramine stay in your system for 6-8 hours - sometimes longer. They don’t just help you fall asleep; they linger and interfere with your natural wakefulness cycle. That’s why you feel foggy, slow, or uncoordinated the next day. It’s not just tiredness - it’s a drug effect.
Can OTC sleep aids cause addiction?
They don’t cause physical addiction like opioids or alcohol, but they can create psychological dependence. Many people feel they can’t sleep without them. Stopping often leads to rebound insomnia - where sleep gets worse than before. This makes people keep using them, even when they know it’s not healthy.
What’s the best alternative to OTC sleep aids?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold standard. It’s as effective as medication - without side effects - and the results last. Other helpful changes include getting morning sunlight, avoiding screens before bed, keeping a consistent sleep schedule, and only going to bed when sleepy. These work better than any pill.
Jay Tejada
January 5, 2026 AT 05:03Been using diphenhydramine for years ‘cause my brain won’t shut off. Didn’t realize I was basically doping myself with allergy medicine. Guess I’ll try that CBT-I thing now-might as well not turn into a dementia statistic by 60.
Allen Ye
January 5, 2026 AT 20:08It’s fascinating how we’ve outsourced our biological rhythms to pharmaceutical convenience. We live in a culture that pathologizes normal wakefulness, then medicates the symptom without addressing the root-chronic stress, digital overstimulation, existential dread masked as insomnia. These OTC pills are just modern-day placebo rituals, wrapped in the false comfort of ‘natural’ labels and pharmacy branding. We don’t need more chemicals; we need to reclaim silence, darkness, and the courage to sit with our own minds at night.
josh plum
January 6, 2026 AT 17:16They don’t want you to know this, but Big Pharma secretly owns the melatonin market. That’s why the labels are so wildly off-because they’re testing how much you’ll swallow before you catch on. And don’t get me started on CBT-I. It’s a government-funded distraction so you don’t sue them for causing your sleep problems with EMF, fluoridated water, and 5G. You think your insomnia is stress? Nah. It’s the chemicals in your toothpaste.
jigisha Patel
January 7, 2026 AT 08:32The data presented is methodologically sound and aligns with current clinical guidelines. However, the omission of dosage-dependent pharmacokinetics of doxylamine in elderly populations is notable. Furthermore, the assertion regarding melatonin’s unregulated status requires citation of FDA 21 CFR Part 111. The recommendation for CBT-I is valid, yet accessibility disparities in rural India render this intervention inequitable. Structural solutions are preferable to individual behavioral fixes.
Jason Stafford
January 8, 2026 AT 15:05They’re lying to you. Every single one. The ‘two-week limit’? That’s not a warning-it’s a loophole. The FDA allows these drugs because they’re cheap and profitable. But the real reason they’re still on shelves? They’re testing how fast your brain forgets. Once you’re hooked, you’ll blame yourself. Not them. Not the manufacturers. You. And when you finally wake up in a hospital after a fall, they’ll say ‘you should’ve read the label.’ But you didn’t read it because they made it look like candy.
Rory Corrigan
January 10, 2026 AT 11:47It’s funny how we treat sleep like a broken machine you can fix with a screwdriver. We don’t ask why we’re so wired. We don’t ask if our lives are too loud. We just pop a pill and hope the universe resets. Maybe the real cure isn’t CBT-I… maybe it’s learning to be bored again. To sit in the dark. To not chase sleep-but let it find you. 🌙
Connor Hale
January 12, 2026 AT 00:00I used to take melatonin every night for months. Felt like a zombie. Then I just stopped. No withdrawal, no rebound-just quiet. Turns out my brain knew how to sleep all along. I just forgot how to let it. Now I read paper books, keep my phone in another room, and let the dark do its thing. No pills. No guilt. Just sleep.
Catherine HARDY
January 12, 2026 AT 18:22My neighbor’s husband took diphenhydramine for six years. He started forgetting his grandkids’ names. Then he fell in the shower. Then he was diagnosed with early-onset dementia. The pharmacist said it was ‘fine.’ The doctor said ‘it’s common.’ No one said ‘it’s killing him.’ I don’t trust anything that comes in a little bottle with a smiling moon on it anymore.