The U.S. Food and Drug Administration doesn’t just approve drugs and medical devices - it watches them after they’re on the market. That’s where MedWatch comes in. It’s not a flashy program, but it’s one of the most important tools keeping patients safe. Every year, over a million reports of side effects, malfunctions, and dangerous interactions flow into MedWatch. These aren’t just numbers. They’re stories - from a patient who had a rare bleeding episode on a new blood thinner, to a nurse who noticed a pacemaker failing after just six months. And every one of those reports helps the FDA decide whether a product needs a stronger warning, a recall, or even to be pulled off the shelves.
What Exactly Is MedWatch?
MedWatch, officially called the FDA Safety Information and Adverse Event Reporting Program, started in 1993. It’s the FDA’s main way of collecting information about problems with medical products after they’ve been sold to the public. This includes prescription drugs, over-the-counter medicines, vaccines, medical devices like pacemakers or insulin pumps, even cosmetics and hemp-based products. The goal is simple: catch dangers that didn’t show up during clinical trials.
Clinical trials involve thousands of people - but not millions. Rare side effects, interactions with other medications, or problems in older patients with multiple health issues often don’t appear until the product is used by a much larger, more diverse group. That’s where MedWatch fills the gap. It’s not just for doctors. Anyone can report. If you’re a patient, a caregiver, a pharmacist, or even a family member who noticed something unusual after someone took a medicine, you can file a report.
How Does It Work? Two Paths, One Goal
MedWatch runs on two reporting systems. One is mandatory. The other is voluntary. Both feed into the same database - the FDA Adverse Event Reporting System (FAERS), which holds over 28 million reports as of late 2023.
Manufacturers and hospitals have to report. If a company makes a drug or device and learns it might have caused a death or serious injury, they’re legally required to file a report. For deaths, they have 30 days. For serious injuries, they have just five workdays. Hospitals and clinics that use medical devices must also report certain device failures. This is called mandatory reporting, and it’s tracked under Form FDA 3500B.
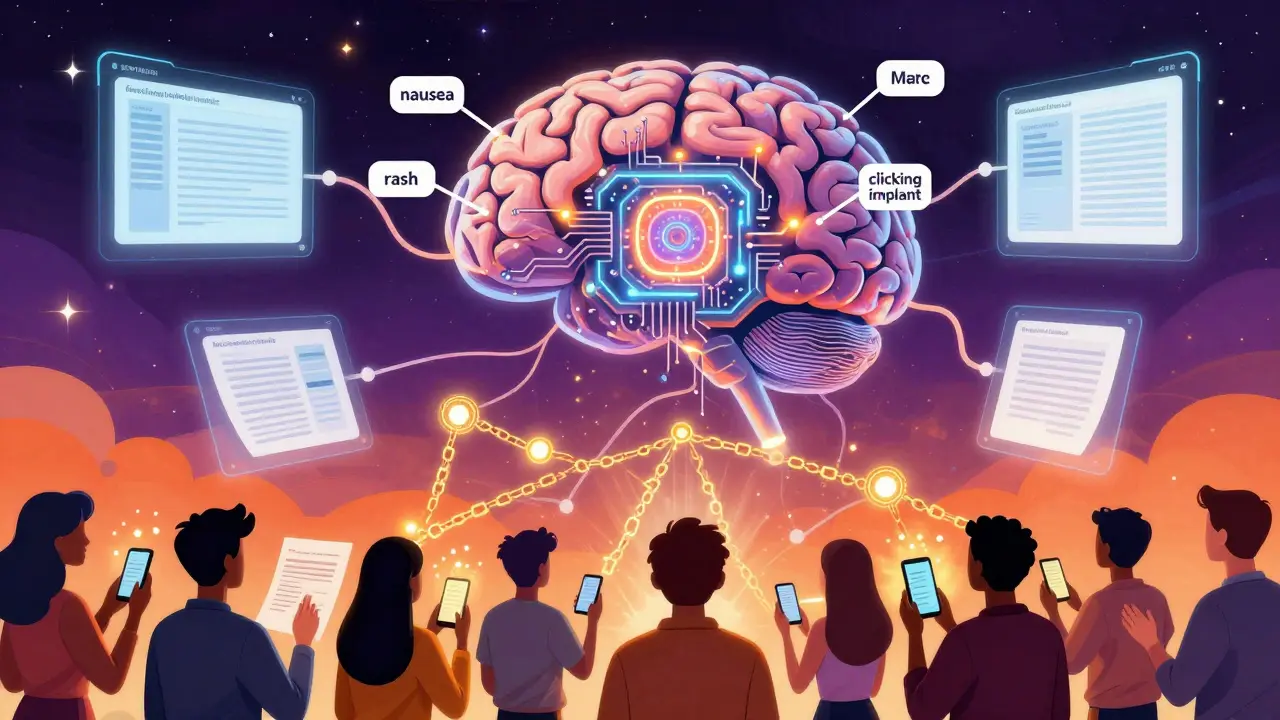
Everyone else uses the voluntary system. That’s Form FDA 3500. You don’t need to be a doctor. You don’t need to prove causation. You just need to describe what happened. Did your blood pressure medicine make you dizzy? Did your knee implant make a clicking sound after three months? Did your child develop a rash after taking an OTC allergy pill? If it’s serious, unusual, or unexpected - report it.
The FDA doesn’t expect you to be an expert. They want details: the name of the product, when you started using it, what symptoms appeared, how long they lasted, and what happened afterward. Even if you’re not sure it was the product’s fault, report it anyway. The FDA’s job is to sort through the noise and find patterns.
What Happens After You Report?
Once a report lands in FAERS, it doesn’t sit there. The FDA uses advanced data tools to scan for signals. Algorithms like the Proportional Reporting Ratio (PRR) and Bayesian Confidence Propagation Neural Network (BCPNN) look for clusters - for example, if 50 people report the same rare liver issue after taking a specific statin, that’s a red flag. The FDA’s Division of Pharmacovigilance reviews about 5,000 potential signals every year.
When a real pattern emerges, the FDA acts. They might update the drug’s label to include a new warning. They might send out a safety alert to doctors and pharmacists. In extreme cases, they recall the product. Take the 2021 recall of Allergan’s BIOCELL textured breast implants. MedWatch reports helped identify a rare cancer link, and within 45 days, the FDA ordered them off the market.
Between 2015 and 2020, MedWatch reports directly led to 37% of all FDA safety communications, according to former FDA Commissioner Dr. Janet Woodcock. That’s not a small number. That’s the difference between a patient knowing about a risk and never finding out until it’s too late.

Who Reports? And Why So Few Do
Here’s the problem: most people don’t report. Studies estimate only 1% to 10% of actual adverse events ever make it to MedWatch. That’s a massive blind spot.
Healthcare professionals are the biggest source of reports - but even they underreport. A 2021 study by the American Medical Association found that most doctors spend 15 to 20 minutes filling out a MedWatch form. That’s time they don’t have. Some electronic health record systems now integrate reporting directly into their workflow, cutting that time to 8-12 minutes. But not all systems do.
Patients face even bigger barriers. A 2022 survey by the National Consumers League found that 68% of people who tried to file a report got stuck on medical jargon. They didn’t know how to describe symptoms accurately. They didn’t know the drug’s brand name or NDC code. Over 40% gave up.
Still, patients are reporting more. In 2022, 42% of reports came from consumers - up from 28% just five years ago. That’s progress. One pharmacist on Reddit shared that 12 reports over five years helped update the label for a blood thinner called Xarelto. That’s real impact.
How to File a Report - Step by Step
If you’ve had a bad experience with a drug or device, here’s how to report it - no medical degree needed.
- Go to www.fda.gov/medwatch. That’s the official portal.
- Click “How to Report” and choose “Consumer or Patient.”
- Fill out Form FDA 3500. You’ll need:
- Name of the product (brand or generic)
- When you started using it
- What happened (symptoms, timing, severity)
- What you did (did you stop the drug? See a doctor?)
- Outcome (did you recover? Was there hospitalization?)
- Your age and sex (optional but helpful)
- Don’t worry if you’re unsure. The FDA says: if you’re not sure, report anyway. They’ll sort it out.
- Submit. You can do it online, fax it to 1-800-FDA-0178, mail it, or call 1-800-FDA-1088.
The FDA offers a free online decision tree tool to help you decide if your event is reportable. It cuts down on incorrect submissions by 38%. Use it.
What’s Changing? The Future of MedWatch
MedWatch isn’t stuck in the past. In September 2023, the FDA launched MedWatch Direct - a new system that lets electronic health records and pharmacy software send reports automatically. Imagine your doctor’s system flagging a possible reaction and sending a report without you lifting a finger.
By mid-2024, the FDA plans to use AI to scan clinical notes for hidden safety signals. Right now, doctors write “patient had nausea after taking lisinopril.” The AI will pull that out, match it to the drug, and add it to the database - even if no one filed a form.
Blockchain is coming too. By late 2024, the FDA wants to verify report authenticity so fake or spam reports don’t clog the system.
But here’s the catch: more technology won’t fix underreporting. The FDA has only 120 staff members analyzing over a million reports a year. Without more people reporting, even the smartest AI can’t find what’s not there.
Why Your Report Matters
MedWatch isn’t perfect. It’s slow. It’s underfunded. It’s confusing for patients. But it’s the only system that gives ordinary people a direct line to the agency that regulates their medicine.
When Dr. Sarah Johnson at MD Anderson reported unexpected immune reactions to Keytruda in 2019, it led to a safety alert within 90 days. That alert saved lives. That report? It came from one doctor who took five minutes to fill out a form.
You don’t need to be a scientist. You don’t need to understand pharmacology. You just need to notice something wrong - and speak up. Because in a system built on data, your voice is the most important signal of all.

Jason Xin
January 29, 2026 AT 15:14Had a cousin on Xarelto who bled out from a minor fall. No one told her the risks. If I’d known about MedWatch back then, I’d have filed a report. Now I tell everyone I know to report weird side effects. It’s not just paperwork-it’s a lifeline.
Donna Fleetwood
January 31, 2026 AT 10:08Seriously, if you’ve ever had a weird reaction to a med or device-just report it. Even if you think it’s ‘nothing.’ The FDA doesn’t need you to be an expert. They just need you to notice something’s off. Your five minutes could save someone’s life.
Melissa Cogswell
February 1, 2026 AT 04:48I work in pharmacy and see patients ignore side effects all the time. They think ‘it’ll go away’ or ‘it’s just me.’ But that’s exactly how patterns get missed. The 3500 form isn’t hard. I print it out for patients who can’t navigate the website. Small effort, big impact.
Diana Dougan
February 1, 2026 AT 22:11Oh wow another ‘your voice matters’ PSA. Congrats FDA, you’ve got 120 people sifting through a million reports while Big Pharma laughs all the way to the bank. And yeah, I’m sure ‘AI will fix it’-right after they fix the fact that your website still uses 2007-era HTML.
Bobbi Van Riet
February 3, 2026 AT 05:52I’ve filed three reports now-two for myself, one for my mom. The first time I tried, I spent an hour trying to figure out if my dizziness was from the blood pressure med or just stress. The FDA’s decision tree helped. It’s not perfect, but it’s the only system that actually listens. I used to think reporting was pointless, but then I read about the Xarelto label change. That came from real people like me. I didn’t know what I was doing, but I did it anyway. And now I feel like I’m part of the solution, not just a patient waiting for the next bad thing to happen.
Sazzy De
February 4, 2026 AT 18:01My knee implant started clicking after 8 months. Told my doctor. He said ‘it’s normal.’ I filed a report anyway. Three months later, the FDA sent out a bulletin. Turns out it wasn’t normal. Just glad I didn’t listen to him.
Blair Kelly
February 6, 2026 AT 02:20Let’s be brutally honest: MedWatch is a joke. Over 28 million reports? Most are garbage. People report headaches from aspirin. They report ‘feeling sad’ after taking vitamin D. The system is flooded with noise, and the FDA’s 120 analysts are drowning. AI won’t fix this-better reporting standards will. Stop encouraging amateurs to file reports. Train the professionals to do it right.
Rohit Kumar
February 7, 2026 AT 06:16In India, we don’t have anything like MedWatch. When a patient has a bad reaction, it’s buried in hospital records or ignored entirely. I wish more people in the U.S. understood how rare this system is. It’s not perfect, but it’s one of the few places where a patient’s voice can actually reach the top. Don’t take it for granted.
Lily Steele
February 8, 2026 AT 18:28My mom took a new statin and got terrible muscle pain. We didn’t know what to do. I found the MedWatch form on my phone during a hospital wait. Took 10 minutes. She’s fine now. No big deal. But I’m glad I did it.
Gaurav Meena
February 9, 2026 AT 01:07As someone who’s seen healthcare systems fail in both India and the U.S., I can say this: MedWatch is a quiet hero. It doesn’t get headlines, but it saves lives. The fact that a grandmother in Ohio can report a side effect and it reaches FDA scientists-that’s revolutionary. Let’s not mock it. Let’s improve it. And let’s teach people how to use it.
Katie and Nathan Milburn
February 10, 2026 AT 22:01According to the FDA’s 2023 annual report, voluntary consumer reports increased by 51% between 2018 and 2023, while manufacturer-reported serious events decreased by 12%. This suggests a systemic shift in reporting behavior, likely due to increased public awareness and digital accessibility. However, the proportionality of signal detection remains statistically inconclusive without normalization by population usage rates.
Beth Beltway
February 12, 2026 AT 01:51Everyone’s acting like this is some noble civic duty. Newsflash: the FDA doesn’t care about your ‘story.’ They care about numbers. And if your report doesn’t fit into a statistical cluster, it gets buried. You think your cousin’s dizziness is ‘important’? It’s noise. The system is broken, and your ‘reporting’ is just emotional theater.
Natasha Plebani
February 12, 2026 AT 17:13The cognitive dissonance here is fascinating. We’re told to report every anomaly as a moral imperative, yet the system is structurally incapable of processing the volume without signal degradation. The BCPNN algorithm, while statistically sophisticated, operates under the assumption of independent, accurate, and complete data inputs-which is patently false. The very mechanism designed to protect us is undermined by the very behavior it incentivizes: unvalidated, emotionally driven reporting. We’ve built a surveillance architecture on the illusion of democratic participation, and now we’re surprised it’s noisy. The real issue isn’t underreporting-it’s epistemic overreach.