Plaque Psoriasis Light Therapy Calculator
Personalized Treatment Estimator
Important: This tool doesn't replace professional medical advice. Always consult your dermatologist before starting treatment.
Living with plaque psoriasis can feel like a nonstop battle: red, scaly patches flare up, itching gets unbearable, and everyday clothing choices become a nightmare. While steroids and biologics dominate the conversation, another option-light therapy-offers a surprisingly gentle and science‑backed way to calm the skin. Below we break down why light therapy for plaque psoriasis is gaining attention, how it works, and what you need to know before you step into the light.
Key Takeaways
- Light therapy (phototherapy) uses specific wavelengths of UV light to slow the rapid growth of skin cells that cause plaques.
- There are three main clinical modalities: narrowband UVB, broadband UVB, and PUVA (Psoralen+UVA). Each has distinct dosing schedules and efficacy rates.
- Clinical trials show 60‑80% of patients achieve at least a 50% reduction in plaque severity after 12‑16 sessions.
- Side‑effects are generally mild-temporary redness or dry skin-but long‑term risks (e.g., skin cancer) are low when treatment follows dermatologist guidelines.
- Home phototherapy units are now FDA‑cleared, providing a convenient alternative for patients who can’t attend weekly clinic visits.
How Light Therapy Works
At its core, light therapy is a treatment that uses ultraviolet (UV) radiation to modulate the immune response in the skin. UV light slows the over‑production of keratinocytes-the cells that pile up to form plaques-by inducing DNA damage that triggers cell‑cycle arrest and apoptosis. It also promotes the synthesis of vitamin D in the epidermis, which helps regulate inflammatory pathways.
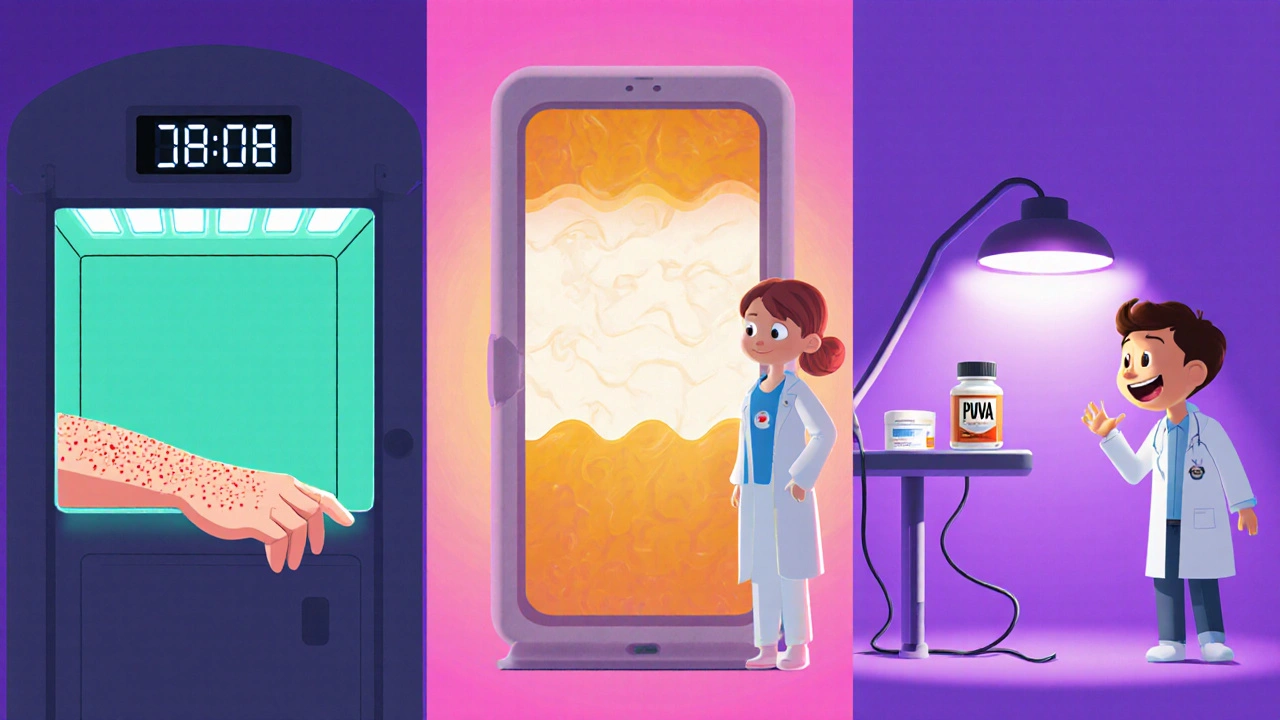
Main Types of Light Therapy for Plaque Psoriasis
Not all UV light is created equal. Dermatologists tailor the wavelength, dosage, and exposure schedule to each patient’s skin type and disease severity.
Narrowband UVB (NB‑UVB)
NB‑UVB emits light at 311‑312nm, a sweet spot that maximizes therapeutic benefit while minimizing burning. Most clinics now favor NB‑UVB because studies report a 70‑80% improvement rate after 20‑30 sessions.
Broadband UVB (BB‑UVB)
BB‑UVB covers a wider range (280‑320nm). It was the first form of phototherapy approved for psoriasis but tends to require more sessions and carries a slightly higher risk of erythema.
PUVA (Psoralen+UVA)
PUVA combines a photosensitizing drug called psoralen with UVA light (320‑400nm). The drug makes the skin more responsive to UVA, boosting effectiveness for thick, stubborn plaques. However, PUVA involves oral medication and has a higher cumulative skin‑cancer risk, so it’s usually reserved for severe cases.
Excimer Laser (308nm)
The excimer laser delivers a focused beam of 308nm light directly to plaques, allowing higher intensity without affecting surrounding skin. It’s ideal for isolated lesions but can be costly.
Home Phototherapy Units
Modern home devices are FDA‑cleared narrowband UVB units that patients can use under a dermatologist’s supervision. They mimic clinic dosing schedules, offering flexibility for busy lives. A typical regimen involves 2‑3 sessions per week for 12‑16 weeks.
Effectiveness & Clinical Evidence
Numerous randomized controlled trials back up phototherapy’s potency. A 2023 meta‑analysis of 45 studies found:
- NB‑UVB achieved a 75% mean reduction in Psoriasis Area and Severity Index (PASI) scores after 24weeks.
- PUVA produced the highest median PASI‑75 response (80%), but with a 2‑fold increase in erythema compared to NB‑UVB.
- Excimer laser reached PASI‑90 in 40% of patients with localized plaques after just 10 sessions.
Importantly, many patients maintain improvements for months after discontinuing therapy, especially when combined with moisturizers and mild topicals.
Safety, Risks, and Side Effects
When administered correctly, light therapy is safe. Common short‑term reactions include:
- Redness or mild sunburn (usually resolves in 24‑48hours).
- Dry, itchy skin-easily managed with emollients.
- Temporary darkening of existing tattoos.
Long‑term concerns focus on cumulative UV exposure. Dermatologists track total dosage and limit sessions to keep the lifetime risk of skin cancer comparable to that of moderate sun exposure. For PUVA, the risk rises sharply after >200treatment courses, so clinicians cap the total number of exposures.
Getting Started: Clinical vs. Home Options
Here’s a quick decision guide:
- Visit a dermatologist for an initial assessment. They’ll confirm plaque psoriasis, stage severity, and rule out contraindications (e.g., photosensitivity disorders).
- If you have extensive or severe plaques, in‑clinic NB‑UVB or PUVA is usually recommended first.
- For localized lesions or when travel is challenging, ask about an excimer laser or a home NB‑UVB unit.
- Ensure any home device is FDA‑cleared and comes with a written dosing plan from your doctor.

Practical Tips for Best Results
- Consistency beats intensity. Stick to the prescribed schedule; missing sessions can stall progress.
- Apply a fragrance‑free moisturizer immediately after each session to lock in hydration and reduce peeling.
- Avoid tanning beds and excessive sun exposure during treatment weeks.
- Track your PASI or at least the number of affected body‑surface areas each week to see measurable improvement.
- If you notice persistent redness, scaling, or new lesions, contact your dermatologist; dosage adjustments may be needed.
Frequently Asked Questions
Can I combine light therapy with my current psoriasis meds?
Yes. Light therapy often works synergistically with topical steroids, vitamin D analogues, or systemic biologics. Your dermatologist will adjust dosages to avoid over‑suppression of the immune system.
How long does a typical treatment course last?
Most patients see noticeable improvement after 8‑12 sessions, which usually span 2‑3months. A full course often includes 20‑30 sessions for maximal clearance.
Is light therapy safe for children?
Pediatric phototherapy is practiced, especially for moderate plaque psoriasis. Doses are lower and closely monitored; consult a pediatric dermatologist for a tailored plan.
What are the costs compared to biologic drugs?
A series of clinic‑based NB‑UVB sessions typically costs a few hundred dollars, far less than the annual price of biologics (often >$20,000). Home units have an upfront cost (~$2,000‑$3,500) but become cost‑effective over time.
Can I use light therapy if I have a history of skin cancer?
A prior skin‑cancer diagnosis requires a careful risk‑benefit analysis. Some dermatologists may still prescribe low‑dose NB‑UVB with strict monitoring, while others may steer you toward non‑UV options.
Bottom Line
Light therapy isn’t a miracle cure, but it’s a proven, low‑toxicity option that can dramatically shrink plaques, ease itching, and improve quality of life. Whether you opt for in‑clinic narrowband UVB or a home phototherapy unit, the key is a personalized plan, consistent application, and ongoing dialogue with your dermatologist.

Carl Mitchel
October 15, 2025 AT 19:20Honestly, if you think you can just ignore the downside of UV exposure because it's "gentle," you're living in a fantasy. The skin isn’t a rubber band you can stretch without consequences. Light therapy does help, but only when you respect the dosage limits that dermatologists set. Overdoing it just trades one flare for a future skin‑cancer risk, and that's not a bargain. So, don’t treat it like a free pass to skip other treatments.
Suzette Muller
October 21, 2025 AT 14:13I totally get how overwhelming plaque psoriasis can feel. Light therapy can be a solid middle ground, especially for folks who can't tolerate strong systemic meds. Make sure you keep a daily log of your PASI scores – it really helps you and your dermatologist see progress. And don’t forget a fragrance‑free moisturizer right after each session; it makes a big difference.
Josh SEBRING
October 27, 2025 AT 08:06Sure, phototherapy is cool, but why not just keep slapping on steroids and hope for the best? Everyone acts like UV light is the holy grail, yet the real cure is still out there somewhere. I bet the pharma industry loves this hype.
Lily Tung
November 2, 2025 AT 03:00It should be noted that when one evaluates the utility of narrowband ultraviolet B therapy within the context of contemporary dermatological practice one must consider not only the empirical efficacy data but also the nuanced patient‑specific factors such as Fitzpatrick skin type comorbidities and lifestyle constraints whilst simultaneously acknowledging the inherent limitations imposed by a paucity of longitudinal safety data thereby necessitating a judicious, evidence‑based approach; consequently, the practitioner is obliged to balance therapeutic gain against potential iatrogenic sequelae ensuring that treatment regimens are customized to the individual’s clinical portrait.
Edwin Levita
November 7, 2025 AT 21:53Picture this: a battlefield of inflamed plaques, and then a beam of light swoops in like a heroic spotlight. Yet, the drama doesn’t end there – the skin mourns the loss of its innocence with subtle reddening. Remember, even heroes have flaws; the UV light can betray you if you ignore the dosage warnings. So treat it with the reverence you’d give a temperamental diva.
Xander Laframboise
November 13, 2025 AT 16:46Let's dissect the whole phototherapy narrative, because the superficial hype tends to mask a cascade of complexities that most casual readers simply glide over. First, the distinction between NB‑UVB and BB‑UVB is not just a matter of wavelength but of photobiological response curves that dictate keratinocyte apoptosis rates versus erythema thresholds. Second, the cumulative dose-often expressed in J/cm²-must be meticulously recorded, for each incremental increase carries a non‑linear risk curve for DNA photodamage. Third, the psychosocial dimension cannot be ignored; patients who sense agency over their treatment schedule, especially with home units, report higher adherence and thus better outcomes. Fourth, the synergy with systemic agents is a double‑edged sword; while concomitant methotrexate can modestly enhance UV‑induced immunosuppression, it also amplifies hepatic load, requiring vigilant lab monitoring. Fifth, consider the photoadaptation phenomenon where melanocyte activity can alter skin's responsiveness over successive sessions, necessitating periodic dose recalibration. Sixth, the cost‑benefit analysis varies widely across health systems; in some regions insurance covers clinic‑based NB‑UVB, making it financially viable, whereas in others the upfront capital expense of a home device may be prohibitive despite long‑term savings. Seventh, the risk of premature photoaging-manifested as fine lines and mottled pigmentation-though statistically lower than for sun exposure, still contributes to patient dissatisfaction in the aesthetic domain. Eighth, the specific contraindications such as lupus erythematosus or porphyria demand absolute exclusion, given the potential for catastrophic flares. Ninth, it's paramount to educate patients on adjunctive skin care: barrier‑repair moisturizers applied within 30 minutes post‑exposure can mitigate transepidermal water loss and reduce scaling. Tenth, the compliance factor: missed sessions not only stall therapeutic momentum but can reset the biological clock, forcing clinicians to re‑initiate induction protocols. Eleventh, the emerging evidence on targeted excimer lasers shows promise for recalcitrant plaques, delivering high‑fluence 308 nm photons with spatial precision, though the cost barrier remains high. Twelfth, the genetic predisposition, especially HLA‑Cw6 positivity, may predict a more robust response to phototherapy, hinting at future personalized regimens. Thirteenth, the psychological uplift from visible skin improvement often translates into better mental health scores, underscoring the holistic benefit. Fourteenth, the environmental impact: home units consume modest electricity, presenting a greener alternative to repeated clinic visits. Finally, the overarching message is that phototherapy is not a monolithic treatment but a versatile, modifiable tool that, when wielded with scientific rigor and patient‑centered nuance, can dramatically shift the therapeutic landscape for plaque psoriasis.
Jason Petersen
November 19, 2025 AT 11:40Light therapy works but only if you actually follow the schedule. Skipping weeks just wastes time and money.
Melissa Gerard
November 25, 2025 AT 06:33Sure, just buy a cheap home unit and hope for the best 😒
beverly judge
December 1, 2025 AT 01:26It’s great that you’re considering phototherapy, but remember to keep your skin moisturized after each session to avoid dryness. Also, logging your symptom changes can help both you and your dermatologist track progress. If you ever feel uncertain about the dosage, don’t hesitate to reach out for a quick check‑in.
Capt Jack Sparrow
December 6, 2025 AT 20:20Honestly, I’ve seen NB‑UVB clear up stubborn plaques in just a few weeks when patients stick to the plan. Just make sure you have a solid dosing schedule from your doc and stay consistent. The results speak for themselves if you play by the rules.