Ever wonder why a neck cramp can suddenly bring on a pounding headache? The link between spasms and migraines isn’t a myth-there’s a real physiological conversation happening between your muscles and your brain. This article breaks down what spasms are, how they can ignite a migraine, and what you can do to break the cycle.
What Exactly Is a Spasm?
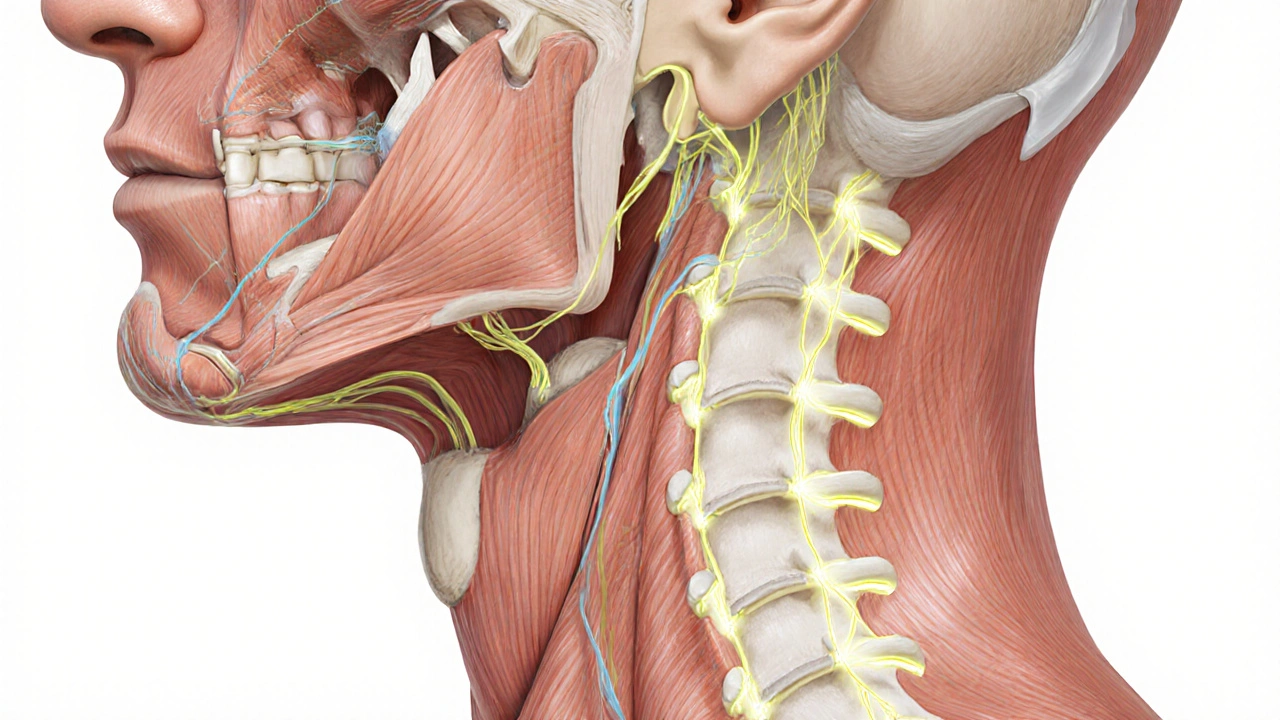
Spasm is a sudden, involuntary contraction of a muscle or group of muscles. It can feel like a tight knot, a twitch, or a painful cramp that lasts seconds to minutes. Common culprits include overuse, dehydration, stress, or an underlying nerve irritation. When a spasm occurs in the neck, shoulders, or head‑related muscles, it often sends pain signals up the spinal cord.
Understanding Migraines
Migraine is a neurological disorder characterized by moderate to severe, throbbing head pain, usually on one side, accompanied by nausea, visual disturbances, or sensitivity to light and sound. While the exact cause remains complex, researchers agree that migraines involve changes in brain blood flow, inflammation of nerve pathways, and abnormal brain activity.
How Muscle Spasms Can Spark a Migraine
The connection boils down to three main pathways:
- Nerve Irritation: A spasm in the cervical spine (the neck) can press on the trigeminal nerve, the main pain conduit for the head. When this nerve is irritated, it can trigger the cascade that leads to a migraine.
- Reduced Blood Flow: Tight muscles compress nearby blood vessels, limiting oxygen‑rich blood to the brain. This hypoxia can set off the vascular component of a migraine.
- Neurochemical Release: Spasms release substances like substance P and CGRP (calcitonin gene‑related peptide) that heighten pain sensitivity and inflammation, both hallmarks of migraine attacks.
In short, a seemingly harmless muscle twitch can act like a domino, nudging the nervous system into a migraine state.
Common Triggers That Link Spasms and Migraines
| Trigger | How It Causes Spasms | Resulting Migraine Mechanism |
|---|---|---|
| Prolonged Screen Time | Forward‑head posture strains neck muscles | Trigeminal nerve irritation → migraine |
| Dehydration | Electrolyte imbalance leads to cramping | Reduced cerebral perfusion → migraine |
| Stress | Elevated cortisol tightens shoulder girdle | Increased CGRP release → migraine |
| Poor Sleep | Muscle recovery is compromised, causing spasms | Fluctuating brainstem activity → migraine |
Diagnosing the Spasm‑Migraine Link
When you visit a healthcare professional, they’ll look for clues that tie muscle tension to your headaches. Typical steps include:
- Physical Exam: The clinician palpates neck and shoulder muscles to locate trigger points.
- Neurological Assessment: Tests reflexes and sensory function to rule out nerve damage.
- Imaging: In some cases, an MRI or CT scan checks for structural issues in the cervical spine.
If the doctor identifies tight trigger points that reproduce your migraine pain, they’ll likely attribute at least part of the headache to muscular factors.
Managing Spasms to Prevent Migraines
Targeting the muscle side of the equation can drastically reduce migraine frequency. Here are evidence‑backed strategies:
- Stretching Routines: Gentle neck rolls, chin tucks, and shoulder blade squeezes performed 2‑3 times daily keep muscles supple.
- Heat Therapy: A warm shower or heating pad relaxes tight fibers and improves blood flow.
- Massage & Trigger‑Point Release: Professional massage or self‑myofascial release with a tennis ball can deactivate painful knots.
- Hydration & Electrolytes: Aim for at least 2L of water per day, and consider magnesium or potassium supplements if you’re a frequent cramp sufferer.
- Ergonomic Adjustments: Raise your monitor to eye level, use a chair with lumbar support, and take a 5‑minute movement break every hour.
Pharmacological Options that Address Both Issues
Some medications help ease muscle spasms while also acting as migraine preventatives. For instance, magnesium citrate relaxes smooth muscle and has modest migraine‑reduction data. In more severe cases, a doctor might prescribe a low‑dose muscle relaxant (e.g., cyclobenzaprine) alongside a triptan for acute migraine relief.
When to Seek Professional Help
If you notice any of the following, it’s time to book an appointment:
- Headaches that worsen with neck movement.
- Spasms that last longer than a few minutes or occur daily.
- Sudden vision changes, weakness, or numbness.
- Any new symptom after a trauma or accident.
Early intervention can prevent the spasm‑migraine cycle from becoming chronic.
Quick Lifestyle Checklist
- Stay hydrated - sip water throughout the day.
- Take micro‑breaks - stand, stretch, and move every hour.
- Prioritize sleep - 7-9 hours on a consistent schedule.
- Manage stress - try breathing exercises or meditation.
- Maintain good posture - align ears, shoulders, and hips.
Frequently Asked Questions
Can a simple neck cramp really cause a migraine?
Yes. A neck cramp can irritate the trigeminal nerve or limit blood flow, both of which are known triggers for migraine attacks. Treating the muscle tension often reduces the severity or frequency of the headache.
Are over‑the‑counter pain relievers enough?
OTC NSAIDs like ibuprofen can help with the pain, but they don’t address the underlying muscle spasm. Combining medication with stretching, hydration, and ergonomic tweaks gives a more lasting solution.
How long does it take to see improvement after changing habits?
Most people notice fewer migraine days within two to four weeks of consistent stretching, hydration, and posture work. Consistency is key; occasional effort won’t break the cycle.
Is massage therapy covered by insurance?
Coverage varies by plan. Some health plans reimburse therapeutic massage if a doctor provides a referral for migraine‑related muscle tension. It’s worth checking your policy or asking the provider.
Can supplements replace prescription meds?
Supplements like magnesium, riboflavin, or CoQ10 can lower migraine frequency for some, but they’re not a guaranteed replacement for prescription preventatives. Talk to a healthcare professional before swapping or adding anything.

Chelsea Kerr
September 28, 2025 AT 05:38Hey there! 🌟 I totally get how a sneaky neck cramp can feel like a thunderstorm in your head. The good news is that simple habits can calm the storm – think regular stretching, staying hydrated, and keeping your screen at eye level. 👀💧 If you notice the pain creeping up after a long day at the desk, try a gentle neck roll for 30 seconds; it often eases the tension that fuels those migraines. Also, a warm compress on the shoulders can boost blood flow and melt the knots. Remember, consistency beats occasional heroics every time. :)
Tom Becker
October 4, 2025 AT 21:38Man, what if the pharma giants don’t want you to know that those “simple” stretches are just a distraction? They’ve been feeding us pills while ignoring the real trigger – hidden EMF waves causing our muscles to spazz out! I’ve seen the docs push meds, but the truth is out there, locked in the spine. Wake up, folks, before they lock us in a cycle of pain and profit.
Laura Sanders
October 11, 2025 AT 13:38Honestly the article overcomplicates a simple neck cramp.
Jai Patel
October 18, 2025 AT 05:38First off, let’s celebrate the fact that you’re even thinking about the connection between muscle tension and head pain, because awareness is the first step toward liberation.
When a spasm in the cervical region is not just a random twitch; it is a signal that the body is screaming for balance.
When the trapezius or suboccipital muscles lock up, they press on the delicate trigeminal pathways, essentially flipping a switch that ignites the migraine cascade.
Imagine your nervous system as a bustling railway station, and a tight muscle as a stubborn gate that blocks the flow of trains, causing a traffic jam of pain signals.
That blockage forces the brain to reroute blood, leading to hypoxia, which in turn fuels the throbbing that migraine sufferers dread.
Research from leading neurology labs has shown that sustained contraction releases neuropeptides such as CGRP, a notorious culprit in migraine inflammation.
Therefore, targeting those peptides through dietary magnesium or professional massage can be as effective as a prescription in many cases.
In practice, a daily routine of six neck rotations, ten chin tucks, and two shoulder blade squeezes, performed with mindful breathing, can rewrite the script of chronic pain.
Couple this with a hydration plan that guarantees at least two liters of water plus a pinch of electrolyte tablets, and you’re giving your cells the fuel they need to stay relaxed.
Ergonomics also play a starring role; raise your monitor, sit with lumbar support, and stand up every hour to break the static load.
If you have the luxury of a yoga mat, incorporate gentle vinyasa flows that stretch the anterior chain and release the posterior tension.
Don’t forget the cultural spice – many ancient Ayurvedic texts prescribe sesame oil massages for exactly this purpose, blending tradition with modern science.
Consistency is key; the brain rewards repeated positive signals, gradually dampening the hyper‑responsiveness that characterizes migraines.
If you ever feel stuck, a quick self‑myofascial release using a tennis ball can dissolve a knot within seconds, granting immediate relief.
So, arm yourself with these tools, stay patient, and watch the frequency of those dreaded migraine days melt away like ice under a summer sun.
Zara @WSLab
October 24, 2025 AT 21:38Great job reading through the science, Zara here! 😊 Remember that small, consistent changes beat big, occasional overhauls. Try setting a timer for a 5‑minute stretch break every hour – it’s amazing how much that can lower migraine triggers. Keep a water bottle on your desk, and don’t forget to breathe deeply when stress spikes. You’ve got this! 🌈
Randy Pierson
October 31, 2025 AT 12:38Nice suggestions! Just a quick note – “lower migraine triggers” could be phrased as “reduce migraine triggers” for smoother flow. Also, “5‑minute” should have a hyphen to link the compound adjective. Your tips are solid and the enthusiasm shines through.
Bruce T
November 7, 2025 AT 04:38Look, we all could do better than ignoring our posture and blaming the world for headaches. Taking responsibility for our own bodies is the only ethical route. If we stop making excuses and start stretching, we’ll cut down on that misery.
Darla Sudheer
November 13, 2025 AT 20:38Totally agree with you Bruce – easy steps like a quick neck roll can make a big difference.
Elizabeth González
November 20, 2025 AT 12:38From a philosophical standpoint, the interplay between muscular tension and neurovascular dynamics underscores the holistic nature of human physiology. When the musculoskeletal system imposes constraints upon cerebrovascular flow, it precipitates a cascade of events that the brain interprets as pain. This phenomenon invites a broader contemplation of the body as an integrated system, wherein localized disturbances can reverberate throughout the entire organism. Consequently, interventions aimed solely at neural pathways may prove insufficient without addressing the peripheral muscular contributors. By embracing an interdisciplinary approach that synthesizes neurology, physiology, and even behavioral science, we may develop more comprehensive strategies for migraine mitigation. Moreover, this perspective aligns with the ancient principle of balance, reminding us that equilibrium must be maintained across all bodily domains to preserve health.
chioma uche
November 27, 2025 AT 04:38THIS IS WHY WE MUST STOP REPEATING WESTERN “ONE‑SIZE‑FIT‑ALL” MEDICAL ADVICE THAT DISRESPECTS OUR NATIVE KNOWLEDGE!
Satyabhan Singh
December 3, 2025 AT 20:38Esteemed colleagues, allow me to elucidate the mechanistic pathway by which cervical musculature influences trigeminal nociception. A sustained contraction induces mechanoreceptor activation, which in turn sensitizes the central pain matrix. The resultant augmentation of CGRP release constitutes a pivotal mediator of vasodilatory processes intrinsic to migraine pathophysiology. Hence, a regimen encompassing precise myofascial release, rigorous postural correction, and judicious supplementation with magnesium can attenuate this cascade. In sum, a multidisciplinary protocol grounded in both empirical evidence and traditional wisdom offers the most robust prophylaxis against spasm‑induced migraine episodes.
Keith Laser
December 10, 2025 AT 12:38Wow, Satyabhan, that was a masterclass in sounding like a textbook. 🙄 But seriously, if we all followed a “multidisciplinary protocol” we’d probably have fewer migraine‑related meltdowns. Maybe sprinkle some humor in the guidelines so people actually read them.
Winnie Chan
December 17, 2025 AT 04:38Sure, because a 5‑minute stretch will totally solve all my migraine problems, right?