Proton Pump Inhibitors and Nexium: What’s Really Going On?
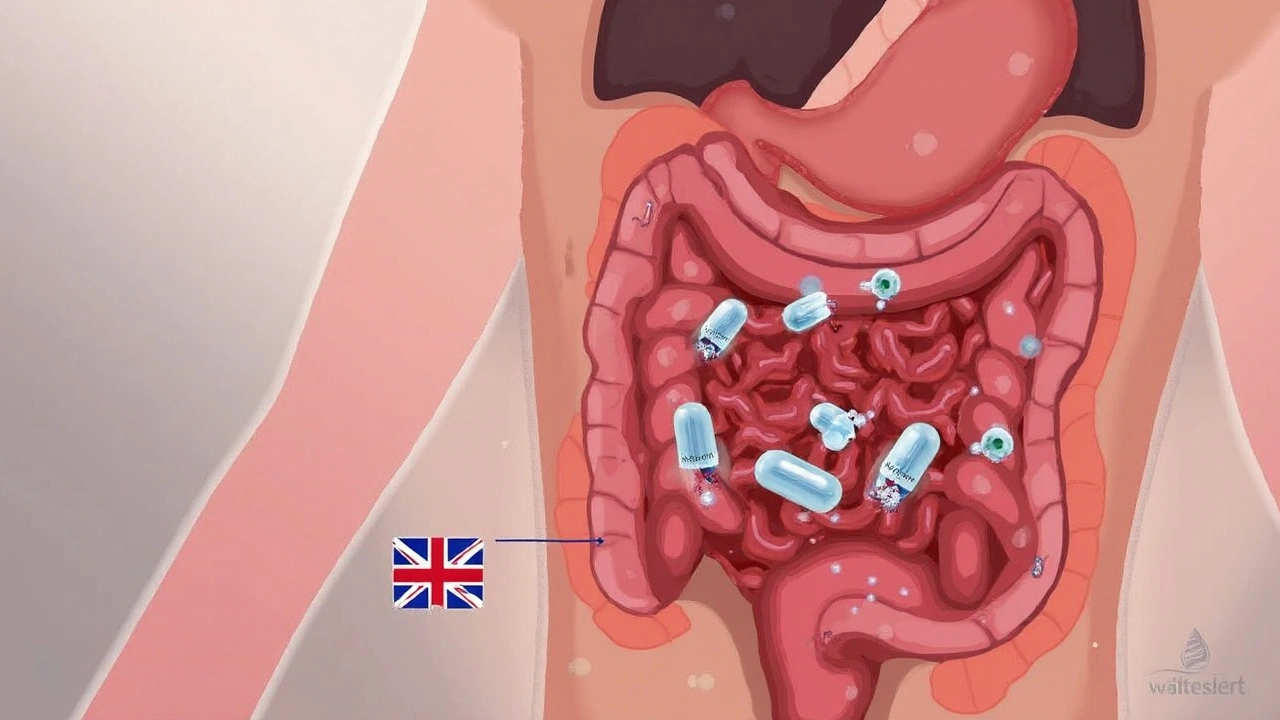
If you’ve ever struggled through that burning acid in your throat after dinner or wondered how your friend can guzzle coffee with no problem, you’ve probably heard about Nexium, sometimes called the “Purple Pill.” Science class in high school probably didn’t cover what a proton pump was, but in your stomach, these pumps are constantly at work. Their job? Moving acid from the cells lining your stomach into the space where it helps digest that burger you had for lunch. Too much acid though, and suddenly dinner feels like a mistake. Esomeprazole—the main ingredient in Nexium—steps in by latching onto those proton pumps, shutting them down before they spray too much acid everywhere. That’s what gives these pills their name: proton pump inhibitors, or PPIs.
Why does this matter? Well, acid is a bit of a double-edged sword. It’s awesome at breaking food down, keeping your stomach healthy, and even wiping out some bacteria before they get into trouble. But it becomes a problem when it starts creeping up into places like your esophagus, leading to heartburn or the full-on misery of GERD (gastroesophageal reflux disease). Nexium works by targeting the final stage in acid production. Rather than just soaking up excess acid (like old-school antacids), it prevents a good chunk—up to 90–95%—from ever being made. This is why doctors love PPIs for long-term reflux control—when you need more than a quick fix.
Here’s something a lot of people don’t realise: you actually have to take esomeprazole a bit before you eat, usually 30 to 60 minutes prior. Why? The pumps need to be active and accessible for the drug to block them. Ever notice you get better results if you time your dose just right? It’s not in your head.
Nexium has another trick: it’s actually considered a ‘cleaner’ version of omeprazole (another popular PPI), meaning your body absorbs and uses it a bit differently. Some research shows it might stick around a little longer or act a bit stronger for some folks. That’s why people sometimes try Nexium if other PPIs aren’t cutting it.
There’s also a little side plot with genetics. Not everyone processes these meds the same. Some people have enzymes that chew through esomeprazole super fast, while others hold onto it longer. This means what works perfectly for your neighbour might not do anything for you—just some scientific weirdness involving your liver and DNA.
Yet, even with all this scientific muscle, PPIs can’t stop every ache. Some people find the effect wears off or doesn’t quite fix those stubborn symptoms. That’s often where the conversation about alternatives comes up—more on that in a bit.
Why the Need for Alternatives?
Ever talked to someone who’s tried half the pharmacy shelf and just can’t get their reflux under control? Or maybe they’re just feeling off after being on Nexium for a while. There’s a reason why not everyone sticks with esomeprazole forever.
The honest truth is, PPIs like Nexium are pretty effective for a big chunk of people. But there are a few real-life headaches that turn up in the doctor’s office, making both patients and doctors start looking for Nexium alternatives.
First, side effects. No one likes to talk about these, but they pop up. The milder ones on Nexium can be stuff like headaches, nausea, or stomach pain. Some people can get diarrhea, or occasionally, constipation. But there are long-term concerns that have gotten more attention lately, like whether taking PPIs for years can mess with your magnesium levels, your risk for certain gut infections, or even your bones. A decent-sized Australian study in 2022 found that people on high-dose PPIs long-term had a slightly higher risk of broken bones, especially women over 60. Now, the increase wasn’t wild, but it’s the sort of thing you want to know if you’re planning to be on one of these drugs for years.
Then there’s the issue of “rebound acid hypersecretion.” Basically, when you stop a PPI like Nexium suddenly, your stomach can go into acid production overdrive. You drop the meds, and suddenly you’re swimming in more acid than you ever thought possible. It’s not dangerous, but it does make quitting cold-turkey really uncomfortable, almost like your symptoms are worse than ever.
Don’t forget interactions with other medications. Some folks on blood thinners, or meds for their heart, or even depression, can find their drugs don’t work as well if mixed with certain PPIs. Not the kind of thing you want to find out by trial and error.
And finally, sometimes PPIs just don’t do enough. Maybe they help, but there’s still that night-time cough, or they only work if you double up. People find they want more control, fewer pills, or just fewer reminders that their stomach is calling the shots.
When these stories stack up—side effects, rebounding symptoms, not enough relief, or hiccups with other health issues—people start asking about their options. I’ve known mates who just hated waking up with a dry mouth every day or worried about taking something forever. That’s when doctors, pharmacists, and, let’s be honest, Google, all get involved in the hunt for a new plan of attack.
Day-to-Day Life With Nexium: What People Notice
Taking Nexium isn’t just about popping a pill and forgetting about it. For a lot of people, it ends up wrapped into daily routines, from remembering to take it before breakfast to keeping an eye on “trigger foods.” You might have felt that classic relief where, a week in, you finally get through dinner without reaching for an antacid. But other times, folks notice stuff they weren’t expecting.
One thing people commonly notice is how much timing matters. If you take Nexium too far from your meals, it just doesn’t work as well. That’s because the acid pumps need to be “awake” for the drug to block them. I’ve lost count of how many mornings I’ve had where a hectic school run with Thaddeus meant I missed my dose window, only to remember hours later when that familiar burn crept up.
A lot of Australians end up balancing Nexium with lifestyle changes—things like eating smaller meals, sipping chamomile tea, or propping their pillow up to avoid nighttime acid. My wife Hazel swears by late-night snacks of plain yogurt to buffer the stomach. Everyone has their own little tweaks, but the common theme is that one pill rarely solves everything.
Then you get stories from people who, after a while, start feeling “off” in more subtle ways. Maybe it’s tiredness that doesn’t shift, maybe it’s feeling bloated, or the digestive rhythm changing. Not everyone gets this—some folks can stay on Nexium for years with no issues, but enough people feel it that doctors pay attention. It’s probably not in your head if suddenly you’re more sensitive to certain foods, or find yourself craving salty things (since PPIs can sometimes throw off sodium and magnesium levels).
There’s also this weird side effect very few mention: an increase in respiratory infections. Australian research teams out of Melbourne found that regular PPI users have a slightly higher chance of picking up some chest colds. The theory is that less stomach acid means more bacteria sneak through. Doesn’t mean you’ll always get sick, but it’s one more thing to keep an eye on, especially during cold season.
One thing I’ve noticed, and a few blokes at the gym have said the same, is when you finally try to cut back or stop Nexium, those symptoms can return with a vengeance for a week or two. It’s a wild cycle most people don’t expect, and it sometimes makes switching trickier than it seems on paper.
Switching Medications: How and Why
So what actually pushes someone to try something besides Nexium? Sometimes it’s medical, other times it’s quality of life, or even just plain curiosity. Here’s what I’ve seen, and what the research is starting to show.
For starters, different PPIs work just a bit differently. There’s esomeprazole (Nexium), but also omeprazole, lansoprazole, rabeprazole, pantoprazole—the names sound confusing, but to your body, each has a slightly different absorption speed, metabolism, and “stickiness” to those acid pumps. Some doctors will switch brands or types just to see if your gut prefers one over the other. This is pretty common, and usually safe with your doctor’s supervision.
Then there are the H2 blockers, like ranitidine (at least, before they pulled it from shelves due to impurities) or famotidine. These work a couple steps earlier in the acid cycle—think of them as the “middle management” of acid blockers. They’re usually less potent than PPIs, but don’t cause rebound symptoms as sharply, so people sometimes switch if they’re looking to taper off.
A lot of patients talk about wanting less pill dependency, especially after reading online about long-term PPI use. Some want to see if their GERD or reflux can be controlled with lifestyle tweaks alone: things like losing weight, quitting smoking, eating dinner earlier, or wearing loose pants. Others like to try non-drug “natural” approaches—herbal teas, supplements, or seeing if probiotics help.
Allergic reactions crop up too, though they’re rare. Maybe someone just can’t tolerate the original PPI, breaks out in hives, or gets nasty headaches that never go away. That’s enough to make anyone look for alternatives. Other folks worry about how their heart meds interact with PPIs. For example, people on clopidogrel (a blood thinner) sometimes get told to avoid certain PPIs because of metabolic snags.
Occasionally, you’ll see a patient whose insurance or pharmacy just stops carrying their PPI, or changes the price suddenly. Aussies might get a script for a generic version, and find it works slightly differently in their system. All these things add up to a lot of trial and error.
If you’re curious about the full menu of options, here’s a handy place to start: Nexium alternatives.
Of course, it’s never wise to swap or stop medications on your own—always loop your doctor in on your plans. But it’s totally normal to want to know your options, especially if something just isn’t working right. A quick chat at your next GP appointment can open the door to trying something that might better fit your lifestyle, your biology, or just your wallet.

Making the Most of PPIs: Tips for Getting Results (and Staying Safe)
If you’ve landed on a PPI like Nexium, getting the most out of your prescription (and avoiding the annoying surprises) isn’t complicated, but there are a few tricks that make life easier. First off, timing is everything. Take your pill 30 to 60 minutes before your first main meal—breakfast, for most of us. This is when acid pumps are primed and ready for that “off” switch. Work it into your morning ritual: right after brushing your teeth, maybe, so you don’t forget.
Eat consciously. It’s not just about the drug—what you eat can tip the acid balance, too. Watch out for the usual suspects: spicy food, tomato sauce, fizzy drinks, alcohol, big dinners late at night. Hazel likes to keep a “trigger diary” where she makes note of foods or habits that set off symptoms for her. It’s surprisingly useful. If you notice, say, that two glasses of white wine plus a curry equals a rough night, you know to steer clear.
Stay hydrated, but try not to guzzle right at mealtime—big gulps can splash acid up the esophagus. Instead, sip between meals. If you deal with nighttime symptoms, raising the head of your bed a few inches (using bricks or a foam wedge, not just an extra pillow) seriously helps. Simple gravity, but you’d be shocked how many people find it’s a game changer.
A warning that bears repeating: don’t stop your PPI suddenly unless your GP gives the okay. If you need to stop or switch, doctors usually use a step-down approach, sometimes adding in an H2 blocker or tapering the dose every few days to reduce the rebound spike. Don’t try cold-turkey unless you’d like to experience acid flashbacks—a mistake I’ve seen too many folks make.
If you’re on Nexium longer than a few months, your doc might order blood tests now and then to check things like your magnesium, B12, or kidney function. A little monitoring goes a long way. If you notice unusual fatigue, muscle cramps, irregular heartbeat, or new digestive issues, flag it for your next appointment—it could be related to the medication.
Here’s a quick look at symptoms and when to seek help:
| Symptom | What to Do |
|---|---|
| Persistent black or bloody stools | Contact your doctor right away |
| Severe abdominal pain | Get medical help quickly |
| Sudden, unintentional weight loss | Don’t wait; notify your doctor |
| Difficulty swallowing | See your GP immediately |
Get to know your body’s signals. Some people find that pairing medications with lifestyle changes keeps symptoms mostly at bay. For others, it’s about checking in every few months to make sure meds are still doing what you need. There’s no failure in switching if something isn’t working—you’re just taking charge.
Navigating acid reflux and meds like Nexium isn’t an exact science. Every person’s mix of biology, habits, and experiences makes the road different. Sharing tips with friends or even your pharmacist can open up solutions you haven’t thought about—sometimes what seems little, like taking your pill the right way or picking a gentler dinner, shifts the whole picture for the better. With a bit of detective work and an open mind, you can find that sweet spot where reflux becomes a background blip, not a main event.

Emily Collier
April 30, 2025 AT 03:56When you first start a proton‑pump inhibitor like esomeprazole, the most important habit is synchronising the dose with your morning routine. The capsule should be swallowed whole with a glass of water at least thirty minutes before breakfast, because the pumps are most active after you eat. This timing maximises the drug’s ability to bind to the H+/K+ ATPase enzyme and prevents the cascade that produces gastric acid. If you miss that window, you’ll often notice a delayed or reduced effect, which can feel like the medication isn’t working at all. Another practical tip is to keep a small pill organizer near your toothbrush so the habit becomes automatic.
Be aware of potential nutrient interactions: long‑term PPI use can impair absorption of vitamin B12, magnesium, and calcium, so periodic blood work is advisable, especially if you have risk factors for osteoporosis. If you experience persistent diarrhea, consider testing for Clostridioides difficile, as reduced stomach acidity can alter gut flora. For patients who develop headaches or a vague sense of fatigue, checking serum magnesium is a quick first step.
Finally, never stop a PPI abruptly. A gradual taper-reducing the dose over two to four weeks or adding an H2‑blocker-helps avoid rebound acid hypersecretion, which can be markedly uncomfortable. Discuss any plan to discontinue with your prescriber, and keep a symptom diary to track whether lifestyle changes are sufficient once the medication is lowered. By combining precise timing, periodic monitoring, and a thoughtful taper, most people can stay symptom‑free without exposing themselves to unnecessary long‑term risks.
Catherine Zeigler
April 30, 2025 AT 03:58One of the things I love about sharing tips on reflux management is seeing how small adjustments can make a huge difference. For example, many folks overlook the power of elevating the head of their bed; even a six‑inch lift can keep nighttime acid at bay and dramatically improve sleep quality. Pair that with mindful eating-avoiding large meals within three hours of bedtime-and you’ll often notice a reduction in both heartburn and that irritating dry cough.
I also recommend tracking trigger foods in a simple notebook; patterns emerge quickly and you can tailor your diet without feeling restricted. Remember, the goal isn’t to eliminate enjoyment but to find balance so you’re not constantly reaching for antacids or fearing your next meal. Keep experimenting, stay patient, and celebrate each small win along the way!
henry leathem
April 30, 2025 AT 04:00The pharmacodynamics of esomeprazole are often overstated in lay articles; the claim that it “shuts down 90‑95% of acid production” glosses over the fact that this inhibition is both dose‑dependent and variable across CYP2C19 genotypes. In practice, the inter‑patient variability can lead to sub‑therapeutic exposure in ultra‑rapid metabolizers, rendering the so‑called “purple pill” ineffective for a non‑trivial subset of the population. Moreover, the rebound acid hypersecretion phenomenon is not merely a nuisance-studies indicate a statistically significant increase in gastric pH oscillations post‑withdrawal, which can exacerbate mucosal injury. Clinicians should therefore consider therapeutic drug monitoring or genotype‑guided dosing rather than relying on a one‑size‑fits‑all protocol.
jeff lamore
April 30, 2025 AT 04:00Good points raised above. It’s also worthwhile to remind patients that taking the medication with a full glass of water helps ensure proper dissolution.
Kris cree9
April 30, 2025 AT 04:01i cant believe ppl still think these pills are magic. sure they help but they also mess w/ your gut flora and can make you feel like a zombie. dont trust every doc who pushes the same old script.
Paula Hines
April 30, 2025 AT 04:02While the anecdotal evidence surrounding PPIs is abundant, it is imperative to acknowledge the empirical data that underscores both therapeutic efficacy and adverse event profiles-particularly the statistically significant correlation between prolonged use and hypomagnesemia. Moreover, the pharmacogenomic variability among individuals necessitates a personalized approach rather than a blanket prescription paradigm. Consequently, clinicians must balance the immediate symptomatic relief against the longitudinal risk factors, ensuring that monitoring protocols are instituted at the outset of therapy
John Babko
April 30, 2025 AT 04:03Listen up, folks! If you’re taking Nexium and still feeling the burn, it’s time to reevaluate your lifestyle choices-cut back on caffeine, avoid late‑night meals, and consider adding an over‑the‑counter antacid for occasional flare‑ups! Also, never underestimate the power of a good sleep posture; a slight incline can work wonders.
Stacy McAlpine
April 30, 2025 AT 04:04That’s solid advice! I’ve found that swapping coffee for herbal tea after dinner and using a pillow wedge really lowered my night‑time reflux. Small changes add up.
Roger Perez
April 30, 2025 AT 04:05🌟 It’s amazing how timing can change the whole game. I started taking my dose exactly 45 minutes before breakfast and the difference is night and day. Also, staying hydrated throughout the day, but not guzzling right before meals, keeps the acid at bay. Keep experimenting and share what works for you! 🌟
michael santoso
April 30, 2025 AT 04:05The discourse lacks critical appraisal of the underlying bias in pharmaceutical marketing. The marginal utility of esomeprazole over generic omeprazole is negligible when scrutinized under cost‑effectiveness analysis, yet the narrative perpetuates a brand‑centric hierarchy that obscures evidence‑based prescribing.
M2lifestyle Prem nagar
April 30, 2025 AT 04:06Stay active, stay positive, and keep tracking your symptoms!
Karen Ballard
April 30, 2025 AT 04:08Great summary! 😊
Gina Lola
April 30, 2025 AT 04:09Sounds legit, I’ll give it a try.
Leah Hawthorne
April 30, 2025 AT 04:10Good info, thanks for sharing.
Brian Mavigliano
April 30, 2025 AT 04:10Really? I always thought the “purple pill” was just a marketing gimmick, but the biochemical nuances tell a different story. Many patients overlook the fact that acid suppression isn’t a binary switch; instead, it follows a sigmoidal dose‑response curve influenced by gastric pH homeostasis, enterochromaffin‑like cell signaling, and even gut microbiota composition. So when you hear someone say they “just take it and forget about it,” that’s oversimplified at best. If you’re not seeing results, consider the CYP2C19 polymorphisms that can render standard doses ineffective-this is why genotype‑guided therapy is becoming more prevalent. And let’s not forget the downstream effects on nutrient absorption; chronic suppression can subtly deplete magnesium and vitamin B12, leading to fatigue that’s often misattributed to other causes. Bottom line: a nuanced, individualized approach beats a blanket prescription any day.
Emily Torbert
April 30, 2025 AT 04:11I totally get how frustrating it can be when the meds don’t seem to help. Maybe try keeping a daily log of what you eat and when you take the pill-sometimes patterns are hidden in the details.
Rashi Shetty
April 30, 2025 AT 04:12While the practical tips are appreciated, it remains essential to acknowledge that long‑term PPI therapy can predispose patients to opportunistic infections, such as Clostridioides difficile, and may interfere with the efficacy of concomitant drug regimens, particularly clopidogrel. 🚩 Regular monitoring and periodic reassessment of the therapeutic necessity are thus paramount.
Queen Flipcharts
April 30, 2025 AT 04:13From a pharmacological perspective, the distinction between esomeprazole and its racemic counterpart is a subtle but important one, influencing both bioavailability and plasma half‑life. Such nuances should inform prescribing habits rather than defaulting to brand loyalty.
Yojana Geete
April 30, 2025 AT 04:14Ah, the drama of acid suppression! One must not merely rely on the chemically‑engineered marvel of the “purple pill,” but also embrace lifestyle harmonies-think of the body as a grand orchestra where timing, posture, and even the moon’s phase can dictate the symphony of digestion.
Jason Peart
April 30, 2025 AT 04:15Hey everyone, just wanted to say that whatever path you take-whether it’s staying on Nexium or exploring alternatives-remember you’re not alone. If you hit a snag, drop a comment and we’ll troubleshoot together. Keep your chin up!