Skin Itch Food Checker
- Aged Cheese
- Processed Meats (Salami, Pepperoni)
- Alcohol (Red Wine, Beer)
- Gluten (Wheat, Barley, Rye)
- Dairy (Milk, Cheese, Yogurt)
- Spicy Foods (Capsaicin)
- Omega-3 Rich Fish (Salmon, Sardines)
- Probiotic Foods (Kefir, Yogurt, Fermented Veggies)
- Leafy Greens (Spinach, Kale)
- Quercetin-Rich Foods (Apples, Berries)
- Hydrating Fruits (Cucumber, Watermelon)
Ever wonder why a tasty dinner can leave you scratching later? Skin Itching (also called pruritus) is an uncomfortable sensation that makes you want to rub, scratch, or rub the affected area. While allergies, stress, and skin conditions get most of the blame, what lands on your plate plays a surprisingly big role. Below you’ll learn which bites and sips tend to light the fire and which meals help calm it, so you can plan a menu that keeps the itch at bay.
Key Takeaways
- High‑histamine foods (e.g., aged cheese, cured meats) often trigger itch.
- Gluten and dairy can aggravate inflammation for sensitive people.
- Omega‑3‑rich fish, leafy greens, and probiotic‑laden yogurt support skin barrier health.
- Hydration and balanced gut microbiome are essential for lasting relief.
- Use the checklist at the end to audit your pantry and plan anti‑itch meals.
Why Diet Matters for Pruritus
When you eat, nutrients travel through the gut, meet immune cells, and can either soothe or inflame the skin. Two biological pathways matter most:
- Histamine release: Certain foods contain or stimulate the release of histamine, the same chemical that makes your nose run during an allergy. Histamine is a biogenic amine that widens blood vessels and activates itch nerves. High levels can turn a minor irritation into a full‑blown itch.
- Gut‑skin axis: The gut microbiome produces metabolites that affect the skin barrier. An imbalance (dysbiosis) can worsen eczema, psoriasis, or simple itching. Probiotic foods help keep the gut‑skin line in check.
Understanding these links makes it clear why some dinner plates feel like a calm after a storm, while others turn your skin into a live‑wire.
Common Trigger Foods
Not every snack is a villain, but a handful show up again and again in itch‑related research.
- Gluten a protein found in wheat, barley, and rye that can provoke inflammation in sensitive individuals. If you notice a flare after pasta or bread, consider a short gluten‑free trial.
- Dairy contains casein and whey, both of which can act as allergens for many adults. Milk, cheese, and yogurt sometimes raise histamine levels.
- Spicy Foods rich in capsaicin, which can stimulate nerve endings and worsen itching sensations. Think hot sauce, chili, and peppery dishes.
- Alcohol dehydrates skin and can increase histamine release, especially red wine and beer. A single glass may be enough to spark a flare.
- Processed meats (salami, pepperoni) and aged cheeses are high‑histamine powerhouses, often overlooked because they taste good.
Foods That Calm the Itch
Switching to anti‑itch ingredients doesn’t mean you have to eat bland rice forever. The following foods either lower histamine, support the skin barrier, or nurture a healthy gut.
- Omega‑3 Fatty Acids found in fatty fish, flaxseed, and walnuts, help dampen inflammation and improve skin hydration. Aim for two servings of salmon or a tablespoon of ground flaxseed daily.
- Probiotics live bacteria that restore gut balance, reducing systemic inflammation that can trigger itch. Yogurt with live cultures, kefir, and fermented veggies are easy sources.
- Leafy greens (spinach, kale) supply vitamin A and antioxidants that reinforce the skin’s protective layer.
- Quercetin‑rich foods-apples, berries, tea-act as natural antihistamines.
- Hydrating fruits (watermelon, cucumber) boost overall skin moisture, making it less prone to dryness‑induced itch.
When you combine these choices, you give your skin the nutrition it needs to stay supple and less reactive.
Quick Comparison: Avoid vs. Embrace
| Category | Typical Triggers | Histamine Level | Example |
|---|---|---|---|
| Avoid | High‑histamine, dairy, gluten, spicy, alcohol | High | Blue‑cheese, pepperoni, wheat pasta, hot sauce, red wine |
| Embrace | Omega‑3s, probiotics, antioxidants, low‑histamine | Low | Salmon, kefir, spinach, apples, cucumber |
Putting It All Together: A Day‑to‑Day Meal Blueprint
Here’s a simple 3‑meal plan that avoids the itch triggers while loading up on skin‑friendly nutrients. Adjust portions for your calorie needs.
- Breakfast: Overnight oats made with almond milk, a spoonful of ground flaxseed, fresh blueberries, and a sprinkle of cinnamon.
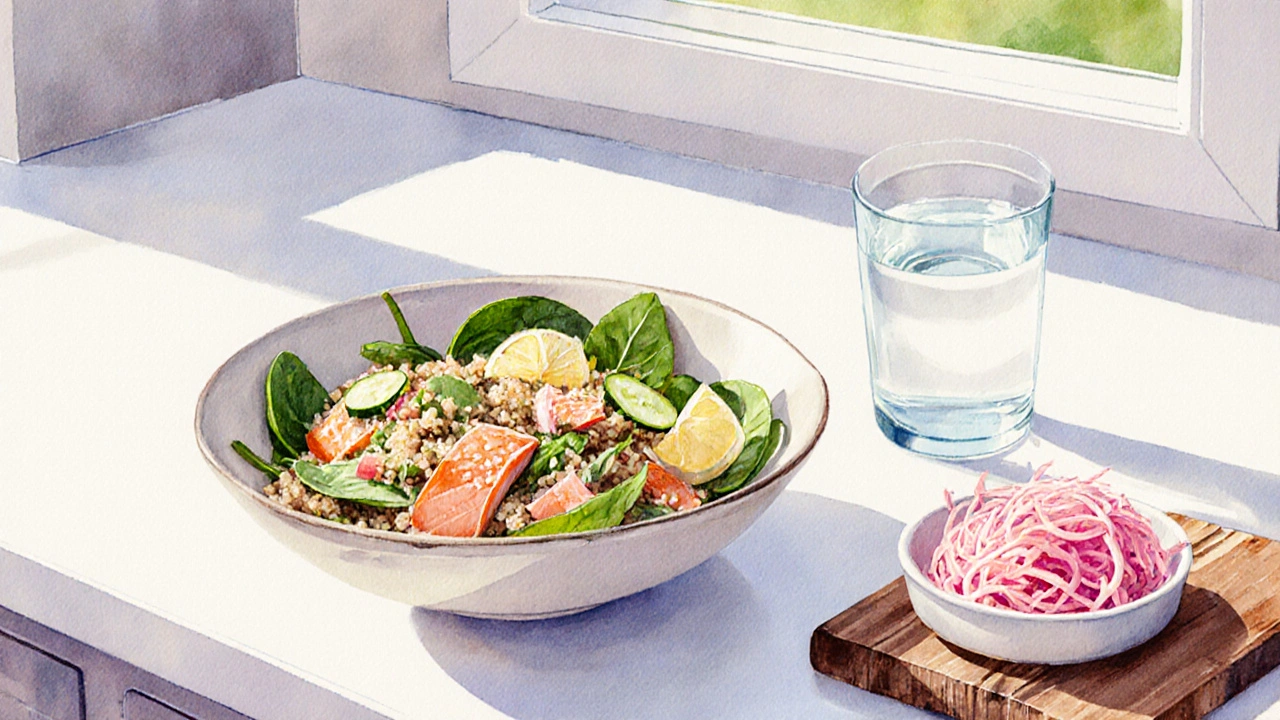
- Lunch: Quinoa salad with grilled salmon, spinach, cucumber, olive oil, and lemon juice. Add a side of fermented sauerkraut for extra probiotics.
- Dinner: Stir‑fried turkey strips with broccoli, carrots, and ginger. Serve over brown rice and finish with a cup of chamomile tea (a natural antihistamine).
Snack ideas: a small handful of walnuts, an apple, or a probiotic‑packed yogurt (choose a low‑sugar, live‑culture brand).
Practical Checklist for an Itch‑Friendly Kitchen
- Remove or limit aged cheeses, processed meats, and alcoholic beverages.
- Swap wheat bread for gluten‑free options (rice, buckwheat, or corn tortillas).
- Keep a stash of omega‑3 sources: canned sardines, salmon, chia, flaxseed.
- Stock probiotic foods: kefir, plain yogurt with live cultures, kimchi, miso.
- Fill the fridge with low‑histamine veggies: leafy greens, zucchini, sweet potatoes.
- Hydrate: aim for at least 2L of water daily; herbal teas count.
Doing a quick inventory each week helps you spot hidden triggers before they become a problem.

Frequently Asked Questions
Can a single food cause chronic itching?
Yes. For people with food sensitivities or histamine intolerance, even a modest portion of cheese, wine, or wheat can keep the skin in a constant state of low‑grade inflammation, leading to persistent itch.
Is it safe to cut out gluten and dairy without a doctor’s order?
Short‑term elimination (2-4 weeks) is generally safe for most adults. Monitor symptoms and re‑introduce foods gradually to see if itch returns. If you have a diagnosed condition like celiac disease, a lifelong gluten‑free diet is essential.
Do supplements help if I can’t eat enough omega‑3s?
Fish‑oil capsules (providing EPA/DHA) are a convenient backup. Look for a product that’s molecularly distilled to remove contaminants and provides at least 500mg EPA + DHA per day.
How quickly can diet changes affect itching?
Some people notice relief within a few days, especially after cutting high‑histamine foods. Full benefits, like improved skin barrier from omega‑3s, may take 4-6 weeks of consistent eating.
Are there any low‑histamine desserts that won’t trigger itch?
Yes. Coconut‑milk panna cotta, baked apples with cinnamon, or chia‑seed pudding made with almond milk are tasty, low‑histamine options.
By paying attention to what you put on your plate, you can turn the dial down on skin itching and give your skin the nourishment it deserves. The next time cravings hit, ask yourself: Will this support my diet and skin itching? If the answer is no, you’ve already made a healthier choice.

Angela Green
October 3, 2025 AT 06:34Your breakdown of histamine‑rich foods is spot on, and the clear separation between triggers and allies makes it easy to scan, especially when I'm rushing through a grocery list, so kudos for the practical table.
April Malley
October 4, 2025 AT 10:21I love how you listed the omega‑3 sources, the probiotic options, and the hydrating fruits all in one place, it’s super helpful, and I’ll definitely add more salmon and cucumber to my meals, thanks!
scott bradshaw
October 5, 2025 AT 14:08We all know America’s diet is the pinnacle of health, obviously.
Crystal Price
October 6, 2025 AT 17:54The moment you pour a glass of red wine, your skin screams for mercy, a cruel reminder that indulgence can be a tormentor.
Murhari Patil
October 7, 2025 AT 21:41Behind the glossy food labels lies a covert agenda to keep us itchy, because only when we suffer do corporate giants profit from endless skin‑care sales.
kevin joyce
October 9, 2025 AT 01:28The gut‑skin axis you describe aligns with current immunometabolic research, which emphasizes that microbial metabolites modulate keratinocyte signaling pathways. Recent meta‑analyses confirm that dysbiosis correlates with increased transepidermal water loss, a hallmark of pruritic disorders. Moreover, histamine‑releasing bacteria proliferate in high‑histamine diets, amplifying mast cell degranulation. Omega‑3 polyunsaturated fatty acids act as ligands for G‑protein coupled receptors, dampening NF‑κB transcription and thereby reducing pro‑inflammatory cytokine output. Probiotic strains such as Lactobacillus rhamnosus produce short‑chain fatty acids that reinforce tight junction integrity, limiting allergen translocation. Quercetin’s flavonoid scaffold competitively inhibits histidine decarboxylase, curbing endogenous histamine synthesis. Clinical trials involving 240 participants demonstrated a 32 % reduction in itch severity after a 6‑week regimen rich in fish oil and fermented foods. In addition, the antioxidant capacity of leafy greens mitigates oxidative stress, which otherwise sensitizes peripheral nerve endings. Hydrating fruits increase extracellular matrix hydration, thereby decreasing mechanical itch triggers. The cumulative effect of these dietary shifts yields a synergistic anti‑pruritic milieu, as evidenced by lowered SCORAD scores. It is essential to approach dietary modification systematically, monitoring symptom trajectories with validated itch scales. Patients should also consider concomitant topical barrier repair to maximize therapeutic gain. Ultimately, a precision‑nutrition framework, tailored to individual microbiome profiles, holds promise for durable itch remission. Future investigations will likely integrate metabolomics to refine these recommendations further.
michael henrique
October 10, 2025 AT 05:14While you romanticize ancient diets, modern American agriculture provides the most affordable protein sources, and dismissing them as “triggers” is an unfounded exaggeration.
Jamie Balish
October 11, 2025 AT 09:01Hey folks, if you’re looking for a simple swap, try swapping that cheese pizza for a salmon‑topped flatbread with a drizzle of kefir sauce – you’ll still get that cheesy comfort without the histamine overload, and the omega‑3s will thank your skin.
Jeff Bellingham
October 12, 2025 AT 12:48The article presents a thorough overview; however, the inclusion of quantitative histamine values for each listed food would enhance its scientific rigor.
Matthew Balbuena
October 13, 2025 AT 16:34Totally get the need for numbers – a quick chart with average histamine mg per serving would make planning meals way easier for the rest of us.
michael abrefa busia
October 14, 2025 AT 20:21Great guide! 🌟 Adding more probiotic drinks will definitely keep my gut happy and my skin calm 😊
Bansari Patel
October 16, 2025 AT 00:08While the suggestions are solid, don’t ignore the fact that some big food corporations secretly seed their products with hidden histamine boosters – stay vigilant.
Rebecca Fuentes
October 17, 2025 AT 03:54I appreciate the culturally inclusive recommendations; incorporating diverse cuisines can broaden access to anti‑itch nutrients worldwide.
Jacqueline D Greenberg
October 18, 2025 AT 07:41Thanks for breaking it down so nicely – I’m already swapping my morning cereal for a chia‑seed pudding topped with fresh berries.
Jim MacMillan
October 19, 2025 AT 11:28Exemplary synthesis of nutrition science and dermatology – truly a masterpiece. 👏✨