Quick Summary / Key Takeaways
- Gene‑editing platforms such as CRISPR are moving from rare dystrophies to age‑related muscle loss.
- Myostatin‑blocking antibodies and ligand traps show promise for sarcopenia and cachexia.
- Stem‑cell and exosome‑based approaches aim to restore the muscle’s own repair engine.
- Most pipelines target delivery challenges with viral vectors, nanoparticles, or hybrid systems.
- Clinical timelines vary: some therapies may be available within 2‑3years, others remain in early‑phase research.
When it comes to skeletal muscle treatments, the next five years could feel like a science‑fiction thriller. Researchers are stitching together DNA, proteins, and tiny vesicles to repair or even rebuild muscle fibers that have been damaged by disease, injury, or aging. This article walks you through the most exciting therapies on the horizon, explains how they work, and gives you a realistic sense of when patients might see them in the clinic.
What counts as a skeletal muscle condition?
Skeletal muscle conditions are a diverse group of disorders that affect the contractile tissue responsible for movement, posture, and metabolism. They include inherited diseases such as Duchenne muscular dystrophy (DMD), acquired ailments like sarcopenia (age‑related muscle loss), inflammatory myopathies, and acute injuries from sports or trauma. The common thread is a breakdown in the muscle’s ability to generate force, sustain itself, or regenerate after damage.
Key metrics clinicians track are muscle strength (measured by grip or leg‑press tests), functional performance (e.g., the 6‑minute walk test), and biomarkers such as creatine kinase levels or circulating myostatin. Understanding these baselines helps researchers gauge how much a new therapy actually improves real‑world function.
Gene‑Based Therapies: Re‑writing the Muscle Blueprint
Gene therapy has graduated from “once‑in‑a‑lifetime miracle” to a viable platform for several rare muscle diseases. The core idea is simple: deliver a functional copy of a missing or defective gene directly into muscle cells.
Viral Vector Delivery (AAV)
Adeno‑associated virus (AAV) vectors are the workhorse for muscle‑focused gene therapy because they efficiently infect non‑dividing cells and provoke a relatively mild immune response. FDA‑approved products like Zolgensma (for spinal muscular atrophy) proved the concept, and now companies are testing AAV‑mediated micro‑dystrophin for DMD. Recent PhaseIII data (2024) showed a 30% increase in the 6‑minute walk distance versus placebo.
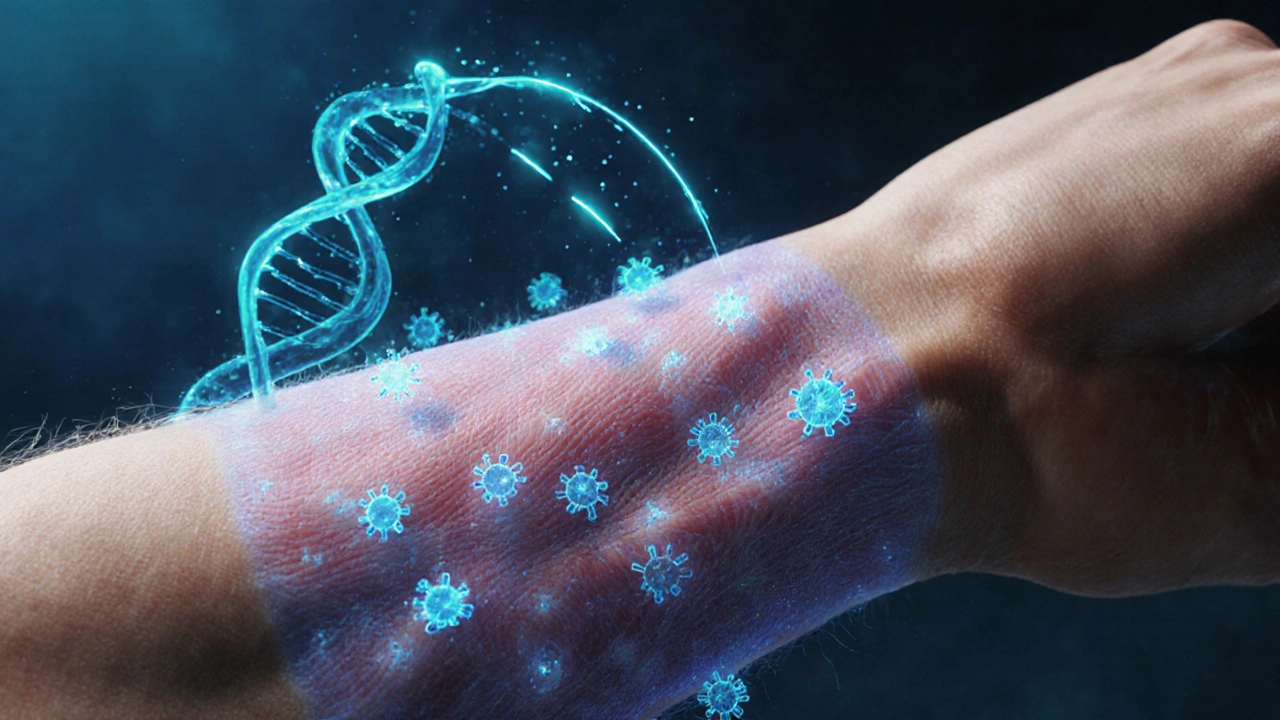
CRISPR‑Cas9 Editing
CRISPR‑Cas9 technology enables precise cuts in the genome, allowing correction of point mutations that cause certain limb‑girdle muscular dystrophies. Early human trials in Italy (2023‑2025) used lipid nanoparticles to deliver CRISPR components to the quadriceps, achieving ~15% editing efficiency and measurable strength gains after six months.
Base and Prime Editing
Beyond cutting DNA, base editors can swap a single nucleotide without creating double‑strand breaks. Prime editing, a newer off‑shoot, expands the range of edits. Although still in pre‑clinical stages for muscle, mouse models of Myotonic Dystrophy type1 showed reversal of toxic RNA foci after a single prime‑editing dose.
Antisense Oligonucleotides (ASOs): Skipping Bad Exons
ASOs are short DNA/RNA strands that bind to specific messenger RNA sequences, prompting the cellular machinery to skip over faulty exons during protein synthesis. The FDA‑approved drug Exondys 51 uses this approach for DMD patients amenable to exon51 skipping. Next‑generation ASOs, such as those targeting exon53 or multi‑exon skipping, are in PhaseII trials and aim to treat up to 80% of DMD genotypes.
Myostatin Inhibition: Turning Off the Muscle Brake
Myostatin (GDF‑8) is a secreted protein that limits muscle growth. Blocking its signaling pathway can yield dramatic hypertrophy in animals. Human trials have focused on two strategies:
- Monoclonal antibodies (e.g., LY‑2495653) that bind myostatin directly.
- Ligand traps such as ACE‑031, a soluble activin‑type II receptor that soaks up myostatin and related ligands.
PhaseII data for ACE‑031 in elderly patients with sarcopenia (2024) showed a 12% increase in thigh muscle cross‑sectional area and modest strength gains. However, off‑target effects on bone metabolism have prompted dose‑optimization studies.
Stem‑Cell and Regenerative Approaches
Muscle contains a resident pool of satellite cells-stem‑like cells that activate after injury. Therapies aim to boost this natural repair system or replace it with exogenous cells.
Autologous Satellite‑Cell Transplant
Patients receive a muscle biopsy, satellite cells are expanded in vitro, and then re‑injected into weakened regions. Small pilot studies in Becker muscular dystrophy reported localized strength improvements, but scaling up remains a logistical hurdle.
Mesenchymal Stem‑Cell (MSC) Infusion
MSC’s immunomodulatory properties make them attractive for inflammatory myopathies. Intravenous infusions of allogeneic MSCs have shown reduced CK levels and improved gait scores in polymyositis patients (PhaseI, 2023).
Exosome‑Mediated Repair
Exosomes are nano‑vesicles packed with micro‑RNA and proteins that can influence muscle regeneration. Pre‑clinical work demonstrated that exosomes derived from engineered MSCs deliver miR‑206, a micro‑RNA that enhances satellite‑cell proliferation. A biotech startup entered a PhaseI trial for post‑stroke muscle weakness in early 2025.
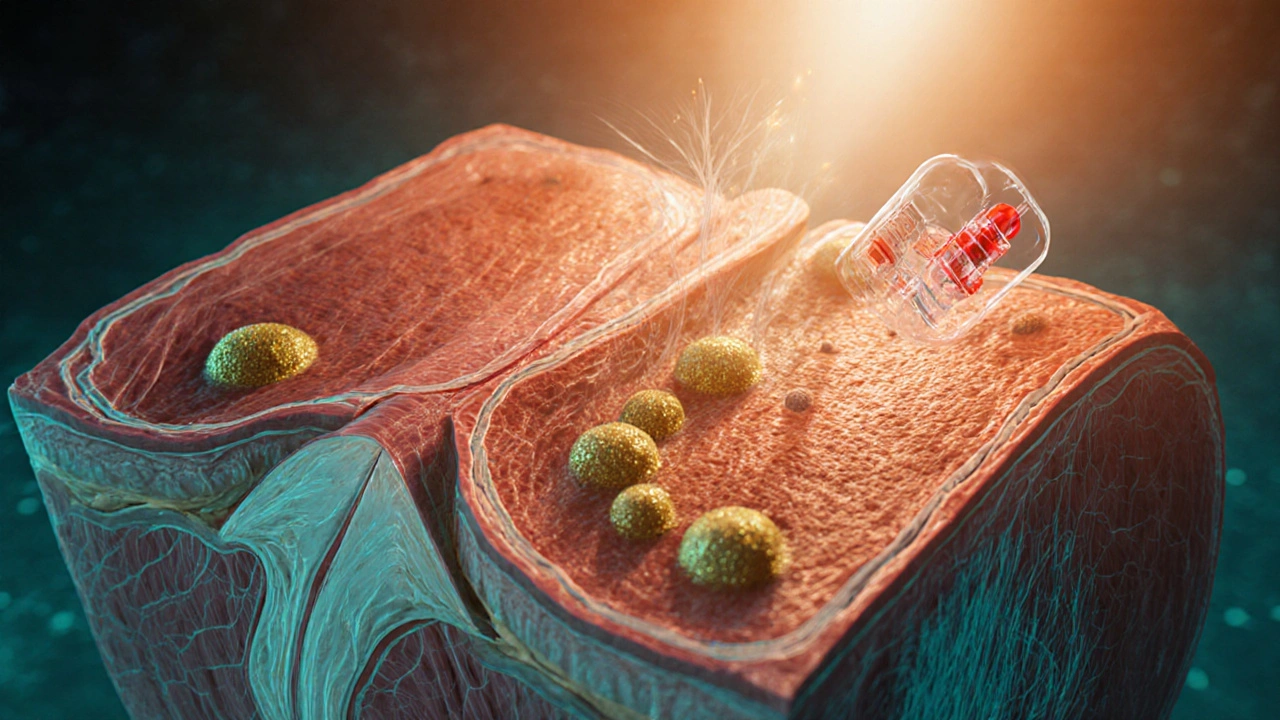
Nanoparticle‑Based Delivery Systems
Getting therapeutic molecules across the dense extracellular matrix of muscle is a major challenge. Researchers are developing lipid‑polymer hybrid nanoparticles that can encapsulate DNA, RNA, or small‑molecule drugs and release them slowly in the target tissue.
One 2024 study showed that a PEGylated nanoparticle carrying a myostatin‑silencing siRNA achieved 80% knockdown of myostatin in mouse tibialis anterior within 48hours, leading to a 20% increase in muscle fiber diameter after two weeks.

Clinical Pipeline Overview: What’s Coming When?
| Therapy | Mechanism | Key Indication | Current Phase | Estimated Market Entry |
|---|---|---|---|---|
| Micro‑dystrophin AAV | Gene replacement | Duchenne muscular dystrophy | PhaseIII | 2026‑2027 |
| CRISPR‑Lipid NP | In‑situ genome editing | Limb‑girdle dystrophy | PhaseII | 2028 |
| Myostatin Antibody (LY‑2495653) | Protein neutralization | Sarcopenia, cachexia | PhaseII | 2027 |
| MSC Exosome Therapy | Paracrine signaling | Post‑stroke weakness | PhaseI | 2029 |
| ASO Multi‑Exon Skipping | RNA splice modulation | Duchenne muscular dystrophy | PhaseII | 2027‑2028 |
The timeline estimates factor in regulatory review, manufacturing scale‑up, and the typical 12‑month gap between successful PhaseIII and market launch. Therapies in PhaseI or II are still several years away, especially those requiring long‑term safety data.
Practical Considerations for Patients and Clinicians
- Eligibility screening: Genetic testing is a prerequisite for most gene‑based interventions. For myostatin blockers, baseline bone density and cardiac function must be evaluated.
- Delivery route: Intravenous infusion works for systemic drugs (e.g., antibodies), while intramuscular injection or regional perfusion is needed for AAV vectors.
- Immune management: Pre‑existing anti‑AAV antibodies can blunt efficacy. Plasmapheresis or immune‑modulating regimens are now standard pre‑treatment steps.
- Cost outlook: Gene therapies currently run in the $1-2million range per patient. Emerging small‑molecule or antibody treatments are expected to be priced lower, though still high compared to conventional drugs.
- Long‑term monitoring: Because many of these therapies are potentially curative, patients will need annual MRI, functional testing, and biomarker panels for at least a decade post‑treatment.
Decision‑Making Checklist for Clinicians
- Confirm genetic diagnosis (if applicable).
- Assess disease stage and functional baseline.
- Evaluate eligibility for each therapeutic class (immune status, organ function).
- Discuss realistic outcome expectations and potential risks.
- Coordinate with a multidisciplinary team (geneticist, physiotherapist, cardiologist).
- Plan post‑treatment monitoring schedule.
Frequently Asked Questions
How soon could gene therapy be available for Duchenne muscular dystrophy?
If the ongoing PhaseIII trials maintain their current success rates, regulatory approval is expected by late 2026, with commercial rollout in 2027. Patients will likely need to enroll in a post‑marketing surveillance program for at least ten years.
Are myostatin inhibitors safe for older adults?
Early studies indicate modest gains in muscle mass, but some participants showed reduced bone density. Ongoing PhaseII trials are testing lower doses combined with calcium/vitaminD supplementation to mitigate this risk.
Can I receive both stem‑cell therapy and an AAV gene product?
Co‑administration is under investigation. The main concern is immune cross‑reactivity; current protocols recommend a wash‑out period of at least six months between the two treatments.
What side effects are common with CRISPR‑based therapies?
The most reported events are transient inflammation at the injection site and mild flu‑like symptoms. Long‑term off‑target edits are a theoretical risk, but deep‑sequencing of treated tissues so far has shown below 0.1% off‑target frequency.
Do exosome therapies require immunosuppression?
Because exosomes are derived from the patient’s own cells (autologous) or from well‑characterized allogeneic sources, they generally do not invoke a strong immune response. Current trials have not required routine immunosuppressants.
Claire Kondash
October 13, 2025 AT 20:11The promise of CRISPR in muscle repair forces us to rethink the boundaries of biology.
When we imagine editing faulty dystrophin genes, we are essentially giving muscles a second chance at life.
Yet the delivery hurdles remind us that even the most elegant code cannot function without a proper vehicle.
Viral vectors, especially AAV, have shown a respectable safety profile, but pre‑existing immunity remains a stubborn obstacle.
Nanoparticle carriers, in contrast, whisper of versatility, slipping through extracellular matrices where viruses stumble.
The ethical dimension deepens as we consider editing somatic cells in elderly patients, raising questions about consent and long‑term effects.
Philosophically, we confront the paradox of prolonging muscle vigor while nature insists on decay.
Are we enhancing humanity or merely postponing an inevitable decline?
The myostatin blockers illustrate how we can amplify natural growth signals, yet they also tip the balance toward unwanted side effects like bone demineralization.
In the realm of stem‑cell therapy, satellite cells are the quiet custodians of regeneration, awaiting a wake‑up call we hope to provide.
Exosome‑mediated delivery, with its cargo of micro‑RNA, offers a subtle way to nudge cellular pathways without overt genetic alteration.
From a practical standpoint, the cost of these technologies continues to hover in the million‑dollar range, a barrier that risks widening health inequities.
Policymakers will need to grapple with reimbursement models that reflect both the upfront price and the downstream savings from reduced disability.
Patient advocacy groups are already lobbying for accelerated pathways, arguing that waiting for perfect data is a luxury many cannot afford.
Ultimately, the convergence of gene editing, protein inhibition, and regenerative medicine may usher in a new era where muscle loss is no longer a guaranteed fate 😃💪.
Pat Mills
October 16, 2025 AT 15:58America’s biotech engine is already outpacing anything the rest of the world can dream of, and the muscle‑focused therapies are the next battlefield.
The sheer scale of US investment in CRISPR and AAV platforms means that the breakthroughs we read about will land on our clinics first.
When European labs stumble over regulatory red tape, American companies barrel forward, turning labs into launch pads.
This isn’t just science; it’s a declaration that we won’t let foreign rivals dictate the future of muscle health.
The next generation of myostatin antibodies will likely bear a red, white, and blue label, showing the world who really leads the fight against sarcopenia.
Ravikumar Padala
October 19, 2025 AT 11:44The hype around gene editing feels a bit overblown when you look at the actual functional gains reported.
Most studies only show modest improvements in walk distance, and those numbers barely move the needle for daily living.
Without a clear path to affordable distribution, these therapies risk becoming another luxury for a few.
In the broader context, we need to ask whether the resources poured into CRISPR could be better spent on proven physiotherapy and nutrition interventions.
King Shayne I
October 22, 2025 AT 07:31i think the real issue isnt the tech its the way pharma pushes these pricey treatments onto patients without proper testing.
theres a lot of hype but also a lot of hidden side effects that get buried in the fine print.
aggressive marketing makes it seem like a miracle, but many dont even know what they are signing up for.
we need stricter oversight before more of these experimental drugs hit the market.
jennifer jackson
October 25, 2025 AT 03:18This is exciting
Brenda Martinez
October 27, 2025 AT 22:04Let me break it down: the pipeline is saturated with glittering promises, yet every new myostatin blocker that hits Phase II ends up a tragic flop.
The data are awash with statistically significant p‑values, but those numbers hide real‑world toxicity that scares off clinicians.
We are being fed a narrative that muscular dystrophy will be cured tomorrow, while the reality is a slow‑moving marathon of failed trials.
If you read between the lines, the entire sector is built on hope sold to desperate families, not on solid, reproducible science.
Marlene Schanz
October 30, 2025 AT 17:51That’s a fair point, and it’s worth remembering that functional outcomes like the 6‑minute walk test can be influenced by many variables.
What’s promising, though, is the incremental gain in muscle cross‑sectional area seen with some exon‑skipping ASOs, which could translate to real strength gains over time.
Combining these molecular approaches with targeted rehab programs might be the sweet spot we need to watch.
Matthew Ulvik
November 2, 2025 AT 13:38Great breakdown! 🎉 The way you laid out the delivery challenges really helps newbies understand why AAV and nanoparticles each have their niche.
If you’re just getting started, focus on the safety data first – the immune‑response profile often decides whether a therapy moves past Phase I.
And don’t forget to keep an eye on the cost‑effectiveness models; they’ll determine how many patients actually get access.
Dharmendra Singh
November 5, 2025 AT 09:24The US does have enormous resources, but it’s also true that our regulatory framework can slow things down just as much as elsewhere.
International collaborations are beginning to share vector designs that could cut down on redundant work.
In the end, a balanced global effort might accelerate approvals more than any single nation acting alone.
Rocco Abel
November 8, 2025 AT 05:11It’s no coincidence that the big pharma giants are all‑in on myostatin blockers right now.
Behind the glossy press releases lies a network of venture capital that thrives on hype cycles, steering research toward profit‑driven endpoints.
One has to wonder whether the observed “efficacy” is sometimes a product of selective reporting rather than genuine therapeutic breakthrough.
Dawn Mich
November 11, 2025 AT 00:58You’re right to call out the unchecked promotion, but let’s not pretend that the scientific community isn’t complicit either.
When trials are funded by the same companies that stand to make billions, the line between rigorous validation and marketing blurs.
It’s a systemic issue that demands stricter conflict‑of‑interest policies across the board.
Eric Sevigny
November 13, 2025 AT 20:44Actually the rehab angle is key – many trials now include a physiotherapy arm to boost the muscle gains from the gene therapy.
There’s evidence that combined approaches can improve the functional scores by up to 20% more than the drug alone.
Just make sure the rehab program is tailored to the patient’s baseline – a one‑size‑fits‑all won’t cut it.
Glenda Rosa
November 16, 2025 AT 16:31“Exciting” is an understatement – the whole field is a kaleidoscope of half‑baked ideas that glitter but rarely deliver.
Until we see long‑term durability beyond a few months, it’s premature to celebrate any of these pipelines.
The market hype is the real muscle here, not the underlying biology.
Aaron Perez
November 19, 2025 AT 12:18Indeed-combining therapeutic modalities-especially when one involves a molecular intervention and the other a physical regimen-creates a synergistic platform that could overcome the limitations of monotherapy!!!
However, the implementation of such integrated protocols demands rigorous standardisation; otherwise, variability in patient compliance could confound the outcome measures!!!
Thus, future trial designs must incorporate precise metrics for both the biological and functional components to truly assess efficacy!!!
William Mack
November 22, 2025 AT 08:04Spot on – safety data will dictate the rollout pace.
Evan Riley
November 25, 2025 AT 03:51The global collab you mentioned might sound noble, but it also opens doors for data leakage and coordinated influence on regulatory bodies.
When the same big players sit at every advisory table, the narrative can be steered toward favorable outcomes, regardless of independent findings.
Nicole Povelikin
November 27, 2025 AT 23:38Sure, because we all trust pharma’s “transparent” reporting…
Michelle Weaver
November 30, 2025 AT 19:11While the concerns raised are indeed valid, it is essential that regulatory agencies enforce stringent conflict‑of‑interest disclosures to preserve scientific integrity 😊.