When you’re managing heart disease, taking multiple pills every day isn’t just inconvenient-it’s a major reason why so many people stop taking their meds. Studies show that when patients have to swallow four or more pills daily, adherence drops to just 25-30%. But what if you could take just one pill instead? That’s the promise of cardiovascular combination generics: single pills that combine two or more heart medications into one easy dose.
What Are Cardiovascular Combination Generics?
These are generic versions of brand-name pills that mix two or more cardiovascular drugs into a single tablet. They’re not new, but they’ve become more common over the last decade. Think of them as the heart version of a multivitamin-except instead of vitamins, you’re getting a statin, a blood pressure med, and maybe an antiplatelet agent, all in one.
The idea started gaining traction after a 2002 study by Dr. Salim Yusuf showed that a single pill containing aspirin, a beta-blocker, an ACE inhibitor, and a statin could cut cardiovascular events by up to 75% in people who’d already had a heart attack or stroke. That’s not just theory-it’s backed by real-world data. A 2020 study in Circulation: Cardiovascular Quality and Outcomes found that if all Medicare Part D patients switched from brand-name combo drugs to generics, the system could save $1.3 billion a year.
Common Drug Combinations You’ll Actually Find
Not every possible combo exists as a generic, but several are widely available and prescribed. Here’s what you’re most likely to see:
- Atorvastatin + amlodipine: A statin for cholesterol + a calcium channel blocker for blood pressure. This combo is sold under brand names like Caduet, but generics are now common and cost under $15 per month.
- Simvastatin + ezetimibe: Two cholesterol-lowering drugs in one pill. The brand version, Vytorin, was expensive. The generic hit the market in 2016 and now costs about 85% less.
- Lisinopril + hydrochlorothiazide: An ACE inhibitor and a diuretic. This combo has been a go-to for high blood pressure for years. Generics are cheap, effective, and widely covered by insurance.
- Metoprolol + hydrochlorothiazide: A beta-blocker and a water pill. Used for hypertension and heart failure. While the brand version (Lopressor HCT) is still around, the generic combo is now standard in many clinics.
- Isosorbide dinitrate + hydralazine: Used specifically for heart failure in Black patients. The brand BiDil became generic in 2012 and remains one of the few race-specific generic combos approved by the FDA.
- Sacubitril + valsartan: A newer combo for heart failure (brand name Entresto). The first generic version was approved in 2022, making this once-expensive treatment much more accessible.
These aren’t just theoretical options-they’re daily reality for millions of patients. In fact, Medicare data from 2017 showed that 43.8% of cardiovascular prescriptions were still for brand-name drugs, even though generics were available. That’s billions of dollars left on the table.
Why Do These Combos Work Better Than Separate Pills?
It’s not just about saving money. It’s about sticking with the treatment.
When you take five separate pills a day, you forget. You run out. You get confused. You feel overwhelmed. But when it’s one pill? Adherence jumps. Studies show that patients on fixed-dose combinations are 15-20% more likely to keep taking their meds compared to those on multiple pills. That’s not a small difference-it’s the difference between preventing a second heart attack and ending up back in the hospital.
One 2020 American Heart Association review found that single-pill combinations improved adherence to 75-85%, compared to just 50-60% for multiple separate pills. That’s why the AHA gives them a Class I recommendation-the highest level of endorsement-for patients who need multiple cardiovascular drugs.
And the cost savings are real. In 2017, the average cost for a brand-name cardiovascular combo was $85.43 per fill. The generic version? $15.67. That’s an 82% drop. For someone on Medicare or without insurance, that’s life-changing.
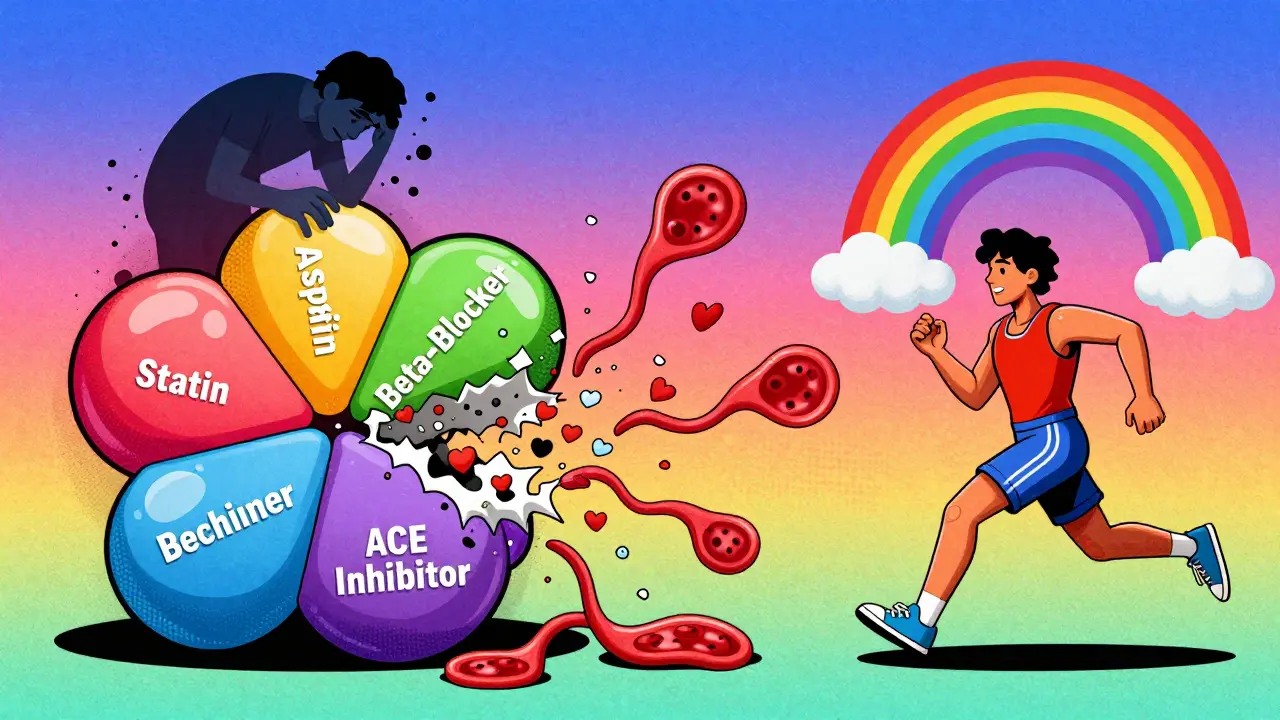
What’s Missing? The Polypill Gap
There’s one combo that’s still rare in the U.S.: the full “polypill.” That’s the one Dr. Yusuf dreamed of-four drugs in one pill: aspirin, a statin, a beta-blocker, and an ACE inhibitor. It’s used in places like India and the UK, where public health programs are pushing it to prevent heart disease in high-risk populations.
But in the U.S., no single pill combines all four. Why? Regulatory hurdles, patent issues, and lack of commercial interest from drugmakers. Even though each component is available as a cheap generic, no company has pushed to combine them into one FDA-approved product. So right now, if you need all four, you’re still taking two or three separate pills.
Some clinics are starting to offer “compounded” versions-pharmacists mixing the pills themselves. But these aren’t FDA-approved, so quality and consistency can vary. They’re an option for some, but not a standard solution.
Are Generics Really as Good as Brand Names?
This is the big question patients ask. And it’s a fair one.
The FDA requires generics to deliver 80-125% of the active ingredient compared to the brand-name drug. That’s a tight range, and it’s backed by decades of data. A 2014 review in the European Heart Journal analyzed 61 clinical trials and found no meaningful difference in safety or effectiveness between brand-name and generic cardiovascular drugs.
But here’s the catch: some patients report side effects when switching. About 12% of patients on Drugs.com noted minor differences-usually with beta-blockers or calcium channel blockers. Why? It’s not the active ingredient. It’s the fillers, dyes, or coatings. For most people, this doesn’t matter. But for those with severe allergies, sensitive stomachs, or narrow therapeutic index drugs (like warfarin), even tiny differences can cause issues.
That’s why experts like Dr. Aaron Kesselheim warn that transitions need care. If you’ve been on a brand-name drug for years and your doctor switches you to a generic, don’t assume everything will be the same. Monitor your blood pressure, heart rate, and symptoms. Talk to your pharmacist. Don’t just accept the change without checking in.
What Are the Alternatives?
If a combination generic isn’t available for your meds, here are your options:
- Take separate generics: This is the most common approach. Instead of a combo pill, you take two or three individual generics. It’s cheaper than brand-name combos and often just as effective. The downside? More pills to remember.
- Use a pill organizer: If you’re taking multiple separate pills, a weekly pill box with morning/evening compartments can help you stay on track. Some pharmacies even offer pre-filled organizers for free.
- Ask about mail-order pharmacies: Many insurance plans offer 90-day supplies of generics through mail-order services. That means fewer trips to the pharmacy and lower co-pays.
- Try a medication therapy management (MTM) program: If you’re on five or more meds, your insurer may offer free counseling from a pharmacist to simplify your regimen. They can flag interactions, suggest combos, and help you cut costs.
And if you’re in a high-risk group-say, you’ve had a heart attack or have diabetes-your doctor might recommend a combination even if it’s brand-name. Sometimes, the cost is worth it if the pill improves adherence enough to prevent a hospital visit.

What Patients Are Saying
On forums like Reddit’s r/heartdisease and PatientsLikeMe, over 1,200 users shared their experiences with generic cardiovascular combos. About 78% said they worked just as well as the brand names. Twelve percent noticed side effects-usually dizziness, fatigue, or stomach upset. But almost all of them said the cost savings made it worth it.
One patient wrote: “I switched from Caduet to the generic. My cholesterol dropped the same, and my blood pressure didn’t budge. But my monthly bill went from $180 to $12. I didn’t even notice a difference-except in my wallet.”
Still, 65% of pharmacists report patients worrying about generics being “weaker.” That’s a myth. The FDA doesn’t approve generics unless they’re bioequivalent. But fear is real. That’s why pharmacist counseling matters.
How to Talk to Your Doctor About Switching
If you’re on multiple heart meds, ask these questions:
- “Is there a generic combination pill that includes all my meds?”
- “If not, can I switch to individual generics to save money?”
- “Are there any of my meds that shouldn’t be switched because of how they’re absorbed?”
- “Can we try a 30-day trial of the generic to see how I respond?”
Don’t be afraid to ask. Many doctors don’t know all the available combos. A 2018 study found only 45% of primary care doctors were familiar with all the generic combination options. You might be the one who knows more than your doctor.
Final Thoughts: It’s Not Just About Cost-It’s About Survival
Cardiovascular disease is the leading cause of death worldwide. And the biggest barrier to saving lives isn’t lack of drugs-it’s lack of adherence. People don’t die because they don’t have access to medicine. They die because they stop taking it.
Cardiovascular combination generics are one of the simplest, cheapest, and most effective tools we have to fix that. They cut costs, simplify routines, and save lives. The science is solid. The data is clear. And the options are growing.
Whether you’re managing high blood pressure, high cholesterol, or heart failure, ask your doctor: Is there a combo pill for me? If not, why not? And what’s the cheapest, most reliable way to get the meds I need-without falling behind?”
Are cardiovascular combination generics as effective as brand-name drugs?
Yes. The FDA requires generic versions to deliver the same active ingredients at the same rate and strength as brand-name drugs, within a strict 80-125% bioequivalence range. Over 60 clinical trials reviewed in the European Heart Journal found no meaningful difference in safety or effectiveness. Millions of patients use these generics daily with the same outcomes as brand-name versions.
Why aren’t there more combination pills available?
Manufacturers rarely develop new combination generics unless there’s strong demand or patent expiration on all components. The full “polypill” (aspirin, statin, beta-blocker, ACE inhibitor) isn’t available as a single FDA-approved generic in the U.S. because no company has pushed for approval-despite its proven potential. Some pharmacies offer compounded versions, but these aren’t regulated like FDA-approved drugs.
Can I switch from a brand-name combo to a generic without risk?
For most people, yes. But if you’re on a medication with a narrow therapeutic index-like warfarin-or have had reactions to fillers in the past, talk to your doctor first. Minor differences in inactive ingredients can cause side effects in sensitive individuals. Monitor your symptoms for the first 2-4 weeks after switching.
What if my insurance won’t cover the generic combo?
Ask your pharmacist for a price check. Many generic combos cost less than $15 a month even without insurance. If your plan denies coverage, your doctor can file a prior authorization or appeal. You can also ask about patient assistance programs through manufacturers or nonprofit groups like NeedyMeds.org.
Do combination generics reduce the risk of heart attacks?
Indirectly, yes. They don’t cure heart disease, but by improving adherence, they significantly lower the risk of future events. Studies show patients on single-pill combinations are 15-20% more likely to take their meds consistently, which translates to fewer hospitalizations and lower death rates. The American Heart Association considers them a Class I recommendation for patients needing multiple cardiovascular drugs.

jesse chen
December 26, 2025 AT 12:07I switched to the atorvastatin + amlodipine generic last year, and honestly? My wallet breathed a sigh of relief. No more $180/month bills-now it’s $12. I didn’t feel any difference in how I felt, just less stress about paying for it. Seriously, why aren’t more people on this? It’s not magic, it’s math.
Also, my pharmacist gave me a free pill organizer-game changer. I used to forget half my meds. Now? I just grab one pill, and done.
Prasanthi Kontemukkala
December 28, 2025 AT 03:50In India, the polypill is actually prescribed by public health clinics-it’s part of our national heart program. One pill, once a day. No one argues about it. It’s just… normal. Here in the U.S., it feels like we’re stuck in some corporate maze where profit > prevention.
I wish more doctors here would just say: ‘Here’s the combo. Take it. Live longer.’ Not a 20-minute lecture on bioequivalence.
Alex Ragen
December 28, 2025 AT 13:23Let’s be honest: this whole ‘combination generic’ movement is just pharmaceutical capitalism repackaged as public health. The FDA’s 80-125% bioequivalence range? That’s a 45% variance window! Do you know what that means? One pill could be 20% stronger than another. And yet we treat generics like they’re interchangeable cookies?
And don’t get me started on ‘compounded’ versions-those are pharmacy alchemy, not medicine. If you’re going to trust your life to a pill, shouldn’t it be standardized? Or are we just too lazy to care about precision?
Lori Anne Franklin
December 28, 2025 AT 18:30OMG I just switched to the lisinopril + HCTZ generic and my co-pay dropped from $75 to $5?? Like… what?? I thought I was being ripped off before but now I feel like a genius.
Also I spelled ‘hydrochlorothiazide’ wrong in my notes like 12 times. I just write ‘the BP water pill’ now. Works fine.
Ryan Cheng
December 30, 2025 AT 12:18If you’re on multiple heart meds and still taking them separately, you’re doing it the hard way. The data is overwhelming: single-pill combos improve adherence by 15–20%. That’s not a ‘nice-to-have’-it’s a survival tool.
And yes, generics work. The FDA doesn’t approve them unless they’re bioequivalent. If your doctor says ‘brand is better,’ ask them to show you the study. Most won’t have one.
Also, ask your pharmacy about mail-order 90-day fills. You’ll save time, money, and headaches. It’s not rocket science-it’s basic healthcare optimization.
wendy parrales fong
January 1, 2026 AT 01:58I used to hate taking pills. Five a day felt like a chore. Then my doctor gave me the simvastatin + ezetimibe combo. One pill. Same results. I started actually remembering to take them. I even set a little alarm. It’s not about willpower-it’s about making it easy.
Life’s too short to fight your meds. Make them work for you, not against you.
Jeanette Jeffrey
January 1, 2026 AT 19:03Wow. Another feel-good article about generics. Let me guess-next you’ll tell me tap water is just as good as bottled. The truth? Some people DO react to generics. I’ve seen it. Dizziness. Fatigue. Heart palpitations. And when you’re on a narrow therapeutic index drug? A 5% difference in absorption can be dangerous.
So stop acting like this is some universal win. It’s not. It’s a cost-cutting measure dressed up as compassion. And the people who suffer the side effects? They’re just told to ‘tough it out.’
Shreyash Gupta
January 2, 2026 AT 23:45Bro, I tried the generic combo after reading this post. Felt weird for 3 days. Like… my chest was heavy? 😔
Went back to brand. Now I feel fine. So maybe generics aren’t for everyone? 🤷♂️
Also, why do Americans care so much about pills? In India, we just eat turmeric and yoga. 😎
Ellie Stretshberry
January 3, 2026 AT 21:20i switched to the generic a few months ago and honestly i forgot about it until my mom asked if i was still taking my heart pills and i was like… wait i only take one now??
no side effects no drama just cheaper and easier. i think its kinda wild that we make something so simple feel so complicated
Zina Constantin
January 4, 2026 AT 19:40As someone who grew up in a country where medicine was scarce, seeing this kind of access in the U.S. still amazes me. We didn’t have combination pills. We had one pill-if we were lucky. So yes, generics aren’t perfect-but they’re a miracle compared to what so many people around the world face.
Don’t let perfect be the enemy of good. One pill that saves your life? That’s not a compromise. That’s progress.
Dan Alatepe
January 5, 2026 AT 06:02yo i took the generic combo and my heart started doing the cha-cha 🫀💃
not joking. felt like my chest was having a rave. went back to brand. now i’m chill again. so yeah-generics ain’t for everybody. my body ain’t a lab rat. i paid my dues with brand name, i ain’t switching back. 💯
Angela Spagnolo
January 7, 2026 AT 04:02I’ve been on the same brand-name combo for 8 years. My doctor said to switch to generic, but I’m scared. What if… I don’t feel the same? What if something goes wrong? I know it’s irrational… but I just… I need to feel safe. Is that so wrong?
I’m not anti-generic. I just… need time.
Sarah Holmes
January 8, 2026 AT 20:38It is an egregious and morally indefensible failure of the American healthcare system that we allow patients to be subjected to the arbitrary whims of pharmaceutical profit margins under the guise of 'cost containment.' The FDA's bioequivalence standard is a mathematical fiction designed to appease corporate lobbyists, not protect human life. To suggest that a 45% variance in pharmacokinetics is acceptable is not only scientifically reckless-it is a form of institutionalized negligence. You speak of 'adherence' as if it were a virtue, when in truth, it is a desperate survival tactic forced upon vulnerable populations by a system that prioritizes balance sheets over biological integrity. The polypill is not a solution-it is a Band-Aid on a hemorrhage.
Kuldipsinh Rathod
January 9, 2026 AT 09:00My dad took the isosorbide + hydralazine combo for heart failure. He’s 72, still walks 3 miles every morning. He says, 'One pill, no fuss.' He didn’t even know it was generic until I told him. He just knows it works.
Why are we making this so hard?